Scientists Identify a Type of Brain Cell That is a Master Controller of Urination

Researchers have identified a subset of brain cells in mice that act as the master regulators of urination.
The research, published as a Reviewed Preprint in eLife, is described by editors as an important study with convincing data showing that oestrogen receptor 1-expressing neurons (ESR1+) in the Barrington’s nucleus of the mouse brain coordinate both bladder contraction and relaxation of the external urethral sphincter.
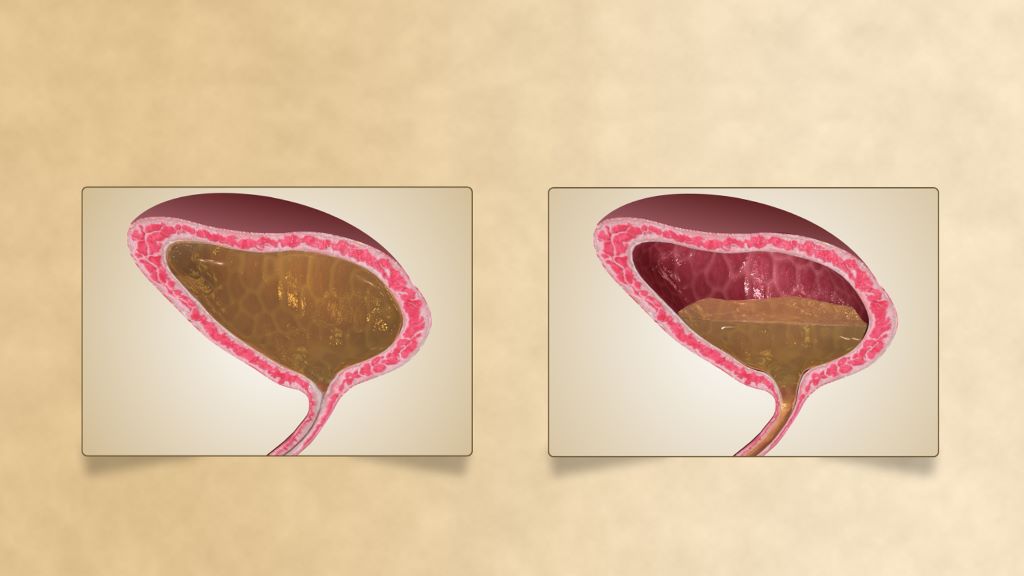
Urination requires the coordinated function of two units of the lower urinary tract. The detrusor muscle of the bladder wall relaxes to allow the bladder to fill and empty, while the external sphincter opens when it’s appropriate to allow urine to flow out, but otherwise keeps tightly shut.
“Impairment of coordination between the bladder muscle and the sphincter leads to various urinary tract dysfunctions and can significantly degrade a person’s quality of life,” says first author Xing Li, Advanced Institute for Brain and Intelligence, School of Physical Science and Technology, Guangxi University, Nanning, China. “But although we know the individual nerve signalling pathways that control each of these urinary tract components, we don’t know which brain areas ensure they cooperate at the right time.”
To explore this, the authors used state-of-the-art live cell imaging to study the activity of brain cells in anaesthetised and awake mice during urination. They focused on a brain region called the pontine micturition centre (PMC), otherwise known as the Barrington’s nucleus, and compared the activity of different PMC nerve cell subtypes.
In their first experiments, they measured the activity of the cells as the bladder empties by measuring changes in levels of calcium. This revealed that the electrical firing rate of a subset of PMC cells expressing estrogen receptors (PMCESR1+ cells) was tightly linked to bladder emptying. When they combined this with monitoring bladder physiology, they found that it was not only the timing of PMCESR1+ cell activity that correlated with bladder emptying, but the strength of cell electrical activity, too.
Next, they tested what happened to urination if they blocked or triggered the PMCESR1+ cells. They found that when PMCESR1+ cell activity was blocked, the amount of urine the mice passed was significantly reduced and ongoing urination was suspended from the moment the cells were inactive. To understand the mechanism behind this, they measured the activity of the bladder muscle and sphincter. They discovered that both increase of bladder pressure and sphincter muscle bursting activity associated with bladder emptying both stopped when PMCESR1+ cell activity was blocked during an ongoing voiding even. Similarly, when PMCESR1+ cells were artificially activated using light, bladder emptying occurred 100% of the time. This suggests that PMCESR1+ cells work as a reliable master switch that either initiates or suspends bladder emptying.
To test whether PMCESR1+ cells can influence bladder emptying independently of controlling the sphincter, they disconnected either the nerve carrying messages from the brain to the sphincter, or the nerve carrying messages from the brain to the bladder. They found that PMCESR1+ cell control of the bladder was fully operational even when communication to the sphincter was blocked, and vice versa. This showed the cells could control the bladder and sphincter independently of one another, but the question remained: could they coordinate the action of the bladder muscle and sphincter together? That is, operate them in a controlled, perfectly timed manner, to trigger bladder emptying when appropriate?
To explore this, they simultaneously recorded bladder pressure and electromyography measurements of sphincter activity. The timing of bladder pressure changes immediately before sphincter bursting activity was consistent for both spontaneous bladder emptying and emptying caused by activating the PMCESR1+ cells, showing that these cells can coordinate the two steps in a precisely temporal sequence and controlled way.
“Our study shows that a subset of cells in the Barrington’s nucleus of the brain can initiate and suspend bladder emptying with 100% accuracy when needed, for example, to release only a small volume for landmarking by animals, or for a human to urinate into a small sample tube for a health check,” concludes senior author Xiaowei Chen, Third Military Medical University, and Chongqing Institute for Brain and Intelligence, China. “While other cells will no doubt be involved in perfect urination control, our pinpointing of PMCESR1+ cells’ crucial role in bladder–sphincter coordination will aid the development of targeted therapies for treating urination dysfunction caused by brain or spinal cord injury or peripheral nerve damage.”
Source: eLife