Point-of-care Ultrasound Enhances Early Pregnancy Care, Cuts Emergency Visits by 81%

Published in Annals of Family Medicine, a University of Minnesota Medical School research team found that implementing point-of-care ultrasounds (POCUS) to assess the viability and gestational age of pregnancies in the first trimester enhanced care for pregnant patients and cut emergency visits by 81% for non-miscarrying patients.
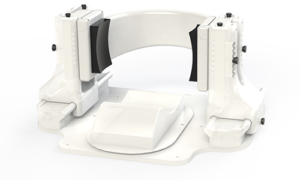
Previously, early pregnancy care was provided through separate appointments for ultrasound, risk assessment and patient education. This new integrated approach allows patients who are under 14 weeks pregnant to receive comprehensive care during a single visit. This includes ultrasound-based pregnancy dating, immediate assessment of pregnancy viability, risk evaluation and on-site counselling – all based on real-time ultrasound results.
“Our study demonstrates that the use of point-of-care ultrasound provides meaningful benefit to the patients we serve by addressing early pregnancy problems at the time they are identified,” said Allison Newman, MD, an assistant professor at the U of M Medical School and family medicine physician at M Health Fairview Clinic. “POCUS in early pregnancy helps clinicians more efficiently and accurately diagnose problems without compromising the quality of needed first trimester assessments – saving time, money and stress for patients.”
The research team introduced this integrated approach at M Health Fairview Clinic – Bethesda in autumn 2022, allowing the clinic to quickly identify high-risk cases and offer timely intervention for issues such as miscarriage or abnormal pregnancies. They found:
- The clinic saw an 81% reduction in emergency visits, urgent clinic appointments and first-trimester phone inquiries for non-miscarrying patients.
- Clinic implementation led to more timely diagnosis of abnormal pregnancies and improved education and support for all patients, including those who experience miscarriage.
- For miscarriage cases, the time from initial concern to diagnosis decreased from an average of 5.8 days to 1.7 days.
Suggested next steps include rolling out the process more widely within other family medicine practices and performing a wider study across multiple sites.
Source: University of Michigan