Head Trauma may Activate Latent Viruses, Leading to Neurodegeneration
In sports, the connection between head injuries and neurodegenerative diseases such as chronic traumatic encephalopathy, Alzheimer’s disease, and Parkinson’s disease is now well recognised.
Researchers at Tufts University and Oxford University have now uncovered mechanisms that may connect the dots between trauma events and the emergence of disease. They point to latent viruses lurking in most of our brains that may be activated by the jolt, leading to inflammation and accumulating damage that can occur over the ensuing months and years.
The results suggest the use of antiviral drugs as potential early preventive treatments post-head injury. The findings are published in a study in Science Signaling.
The microbiome aids in digestion, immune system development, and protection against harmful pathogens.
But the microbiome also includes dozens of viruses that swarm within our bodies at any given time. Some of these can be potentially harmful, but simply lie dormant within our cells. Herpes simplex virus 1 (HSV-1), found in over 80% of people, and varicella-zoster virus, found in 95% of people, are known to make their way into the brain and sleep within our neurons and glial cells.
Dana Cairns, GBS12, research associate in the Department of Biomedical Engineering and lead author of the study, had found evidence in earlier studies suggesting that activation of HSV-1 from its dormant state triggers the signature symptoms of Alzheimer’s disease in lab models of brain tissue: amyloid plaques, neuronal loss, inflammations, and diminished neural network functionality.
“In that study, another virus – varicella – created the inflammatory conditions that activated HSV-1,” said Cairns. “We thought, what would happen if we subjected the brain tissue model to a physical disruption, something akin to a concussion? Would HSV-1 wake up and start the process of neurodegeneration?”
The link between HSV-1 and Alzheimer’s disease was first suggested by co-author Ruth Itzhaki, visiting professorial fellow at Oxford University, who more than 30 years ago identified the virus in a high proportion of brains from the elderly population. Her subsequent studies suggested that the virus can be reactivated in the brain from a latent state by events such as stress or immunosuppression, ultimately leading to neuronal damage.
Blows to Brain-like Tissue
In the current study, the researchers used a lab model that reconstructs the environment of the brain to better understand how concussions may set off the first stages of virus reactivation and neurodegeneration.
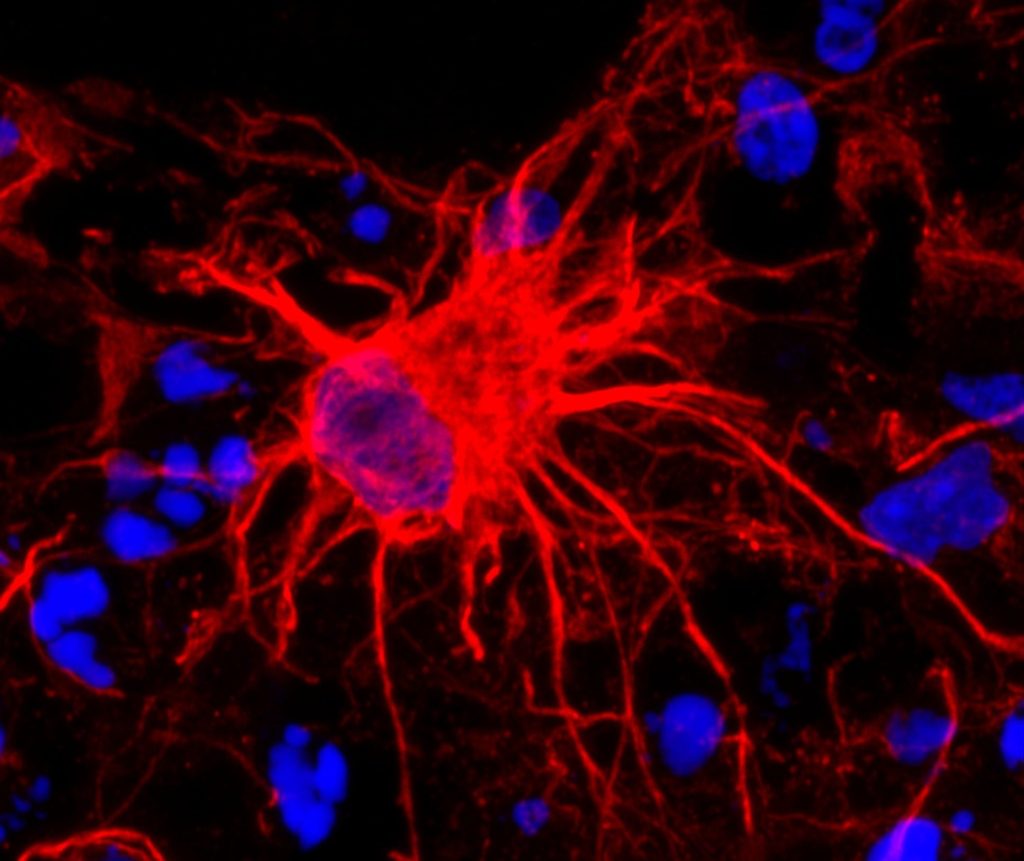
The brain tissue model consists of a 6mm-wide donut-shaped sponge-like material made of silk protein and collagen suffused with neural stem cells, which are then coaxed into mature neurons, growing axons and dendrite extensions and forming a network. Glial cells also emerge from the stem cells to help mimic the brain environment and nurture the neurons.
The neurons communicate with each other through their extensions similarly to how they would communicate in a brain. And just like cells in the brain, they can carry within them the DNA of dormant HSV-1 virus.
After enclosing the brain-like tissue in a cylinder and giving it a sudden jolt atop a piston, mimicking a concussion, Cairns examined the tissue under the microscope over time. Some of the tissue models had neurons with HSV-1, and some were virus-free.
Following the controlled blows, she observed that the infected cells showed re-activation of the virus, and shortly after that the signature markers of Alzheimer’s disease, including amyloid plaques, p-tau (a protein that creates fiber-like “tangles” in the brain), inflammation, dying neurons, and a proliferation of glial cells called gliosis.
More strikes with the pistons on the tissue models mimicking repetitive head injuries led to the same reactions, which were even more severe. Meanwhile, the cells without HSV-1 showed some gliosis, but none of the other markers of Alzheimer’s disease.
The results were a strong indicator that athletes suffering concussions could be triggering reactivation of latent infections in the brain that can lead to Alzheimer’s disease. Epidemiological studies have shown that multiple blows to the head can lead to doubling or even greater chances of having a neurodegenerative condition months or years down the line.
“This opens the question as to whether antiviral drugs or anti-inflammatory agents might be useful as early preventive treatments after head trauma to stop HSV-1 activation in its tracks, and lower the risk of Alzheimer’s disease,” said Cairns.
The problem goes far beyond the concerns for athletes. Traumatic brain injury is one of the most common causes of disability and death in adults, affecting about 69 million people worldwide each year, at an economic cost estimated at $400 billion annually.
“The brain tissue model takes us to another level in investigating these connections between injury, infection, and Alzheimer’s disease,” said David Kaplan, Stern Family Endowed Professor of Engineering at Tufts.
“We can re-create normal tissue environments that look like the inside of a brain, track viruses, plaques, proteins, genetic activity, inflammation and even measure the level of signalling between neurons,” he said. “There is a lot of epidemiological evidence about environmental and other links to the risk of Alzheimer’s. The tissue model will help us put that information on a mechanistic footing and provide a starting point for testing new drugs.”
Source: Tufts University