Bilateral Magnetic Stimulation of the Brain Improves Symptoms of Depression
A type of therapy that involves applying a magnetic field to both sides of the brain has been shown to be effective at rapidly treating depression in patients for whom standard treatments have been ineffective.
Our accelerated approach means we can do all of the sessions in just five days, rapidly reducing an individual’s symptoms of depression
Valerie Voon
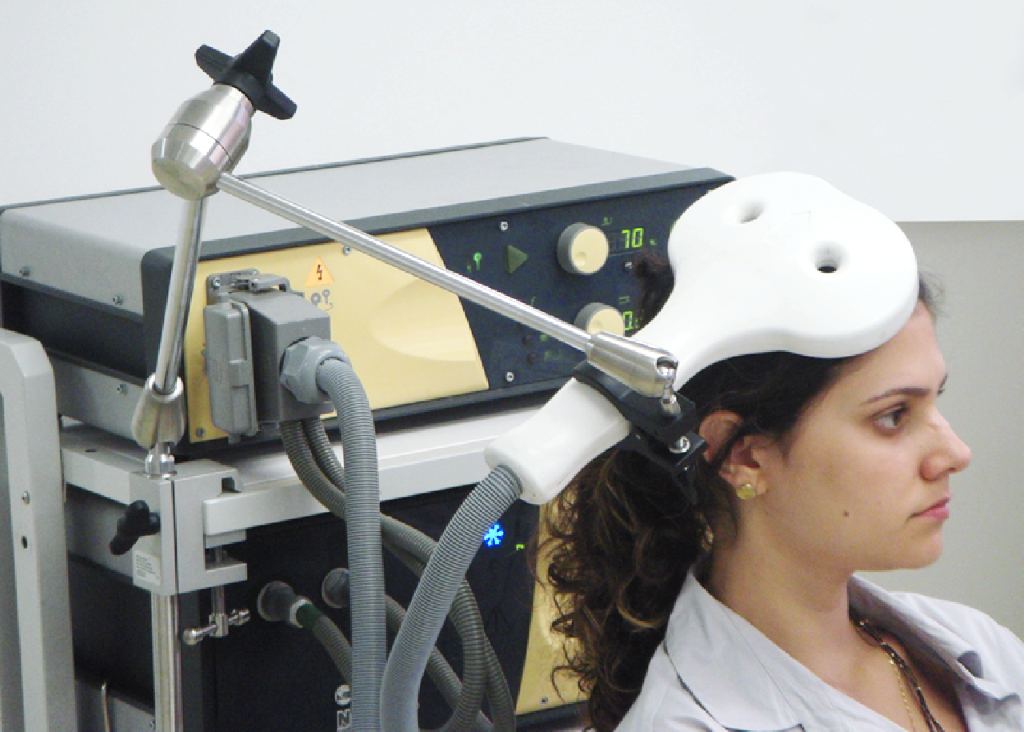
The treatment – known as repetitive transcranial magnetic stimulation (TMS) – involves placing an electromagnetic coil against the scalp to relay a high-frequency magnetic field to the brain.
Around one in 20 adults is estimated to suffer from depression. Although treatments exist, such as anti-depressant medication and cognitive behavioural therapy (‘talking therapy’), they are ineffective for just under one in three patients.
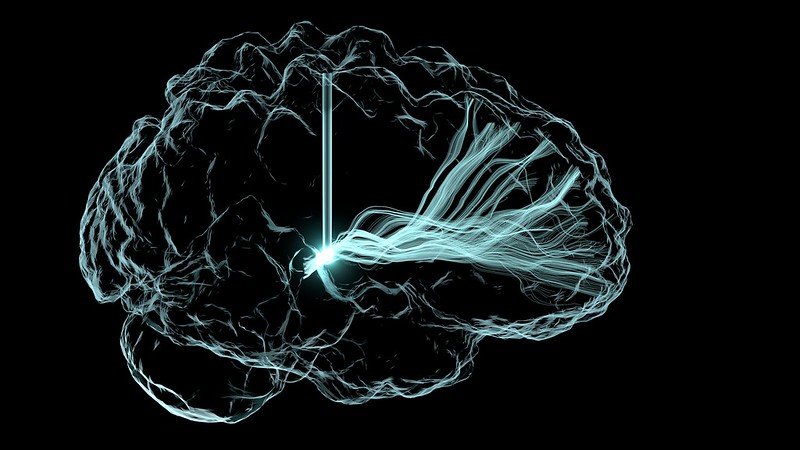
One of the key characteristics of depression is under-activity of some regions (such as the dorsolateral prefrontal cortex) and over-activity of others (such as the orbitofrontal cortex (OFC)).
Repetitive transcranial magnetic stimulation applied to the left side of the dorsolateral prefrontal cortex (an area at the upper front area of the brain) is approved for treatment of depression in the UK by NICE and in the US by the FDA. It has previously been shown to lead to considerable improvements among patients after a course of 20 sessions, but because the sessions usually take place over 20-30 days, the treatment is not ideal for everyone, particularly in acute cases or where a person is suicidal.
In research published in Psychological Medicine, scientists from Cambridge, UK, and Guiyang, China, tested how effective an accelerated form of TMS is. In this approach, the treatment is given over 20 sessions, but with four sessions per day over a period of five consecutive days.
The researchers also tested a ‘dual’ approach, whereby a magnetic field was additionally applied to the right-hand side of the OFC (which sits below the dorsolateral prefrontal cortex).
Seventy-five patients were recruited to the trial from the Second People’s Hospital of Guizhou Province in China. The severity of their depression was measured on a scale known as the Hamilton Rating Scale of Depression.
Participants were split randomly into three groups: a ‘dual’ group receiving TMS applied first to the right- and then to the left-hand sides of the brain; a ‘single’ group receiving sham TMS to the right-side followed by active TMS applied to the left-side; and a control group receiving a sham treatment to both sides. Each session lasted in total 22 minutes.
There was a significant improvement in scores assessed immediately after the final treatment in the dual treatment group compared to the other two groups. When the researchers looked for clinically-relevant responses – that is, where an individual’s score fell by at least 50% – they found that almost half (48%) of the patients in the dual treatment group saw such a reduction, compared to just under one in five (18%) in the single treatment group and fewer than one in 20 (4%) in the control group.
Four weeks later, around six in 10 participants in both the dual and single treatment groups (61% and 59% respectively) showed clinically relevant responses, compared to just over one in five (22%) in the control group.
Professor Valerie Voon from the Department of Psychiatry at the University of Cambridge, who led the UK side of the study, said: “Our accelerated approach means we can do all of the sessions in just five days, rapidly reducing an individual’s symptoms of depression. This means it could be particularly useful in severe cases of depression, including when someone is experiencing suicidal thoughts. It may also help people be discharged from hospital more rapidly or even avoid admission in the first place.
“The treatment works faster because, by targeting two areas of the brain implicated in depression, we’re effectively correcting imbalances in two import processes, getting brain regions ‘talking’ to each other correctly.”
The treatment was most effective in those patients who at the start of the trial showed greater connectivity between the OFC and the thalamus (an area in the middle of the brain responsible for, among other things, regulation of consciousness, sleep, and alertness). The OFC is important for helping us make decisions, particularly in choosing rewards and avoiding punishment. Its over-activity in depression, particularly in relation to its role in anti-reward or punishment, might help explain why people with depression show a bias towards negative expectations and ruminations.
Dr Yanping Shu from the Guizhou Mental Health Centre, Guiyang, China, said: “This new treatment has demonstrated a more pronounced – and faster – improvement in response rates for patients with major depressive disorder. It represents a significant step forward in improving outcomes, enabling rapid discharge from hospitals for individuals with treatment-resistant depression, and we are hopeful it will lead to new possibilities in mental health care.”
Dr Hailun Cui from Fudan University, a PhD student in Professor Voon’s lab at the time of the study, added: “The management of treatment-resistant depression remains one of the most challenging areas in mental health care. These patients often fail to respond to standard treatments, including medication and psychotherapy, leaving them in a prolonged state of severe distress, functional impairment, and increased risk of suicide.
“This new TMS approach offers a beacon of hope in this difficult landscape. Patients frequently reported experiencing ‘lighter and brighter’ feelings as early as the second day of treatment. The rapid improvements, coupled with a higher response rate that could benefit a broader depressed population, mark a significant breakthrough in the field.”
Just under a half (48%) of participants in the dual treatment group reported local pain where the dual treatment was applied, compared to just under one in 10 (9%) of participants in the single treatment group. However, despite this, there were no dropouts.
For some individuals, this treatment may be sufficient, but for others ‘maintenance therapy’ may be necessary, with an additional day session if their symptoms appear to be worsening over time. It may also be possible to re-administer standard therapy as patients can then become more able to engage in psychotherapy. Other options include using transcranial direct current stimulation, a non-invasive form of stimulation using weak electrical impulses that can be delivered at home.
The researchers are now exploring exactly which part of the orbitofrontal cortex is most effective to target and for which types of depression.
The research was supported by in the UK by the Medical Research Council and by the National Institute for Health and Care Research Cambridge Biomedical Research Centre.*
Reference
Cui, H, Ding, H & Hu, L et al. A novel dual-site OFC-dlPFC accelerated repetitive transcranial magnetic stimulation for depression: a pilot randomized controlled study. Psychological Medicine; 23 Oct 2024; DOI: 10.1017/S0033291724002289
*A full list of funders is available in the journal paper.
Source: University of Cambridge. The original text of this story is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Note: Content may be edited for style and length.