South Africa Amended its Research Guidelines to Allow for Heritable Human Genome Editing

Françoise Baylis, Dalhousie University
A little-noticed change to South Africa’s national health research guidelines, published in May of this year, has put the country on an ethical precipice. The newly added language appears to position the country as the first to explicitly permit the use of genome editing to create genetically modified children.
Heritable human genome editing has long been hotly contested, in large part because of its societal and eugenic implications. As experts on the global policy landscape who have observed the high stakes and ongoing controversies over this technology — one from an academic standpoint (Françoise Baylis) and one from public interest advocacy (Katie Hasson) — we find it surprising that South Africa plans to facilitate this type of research.
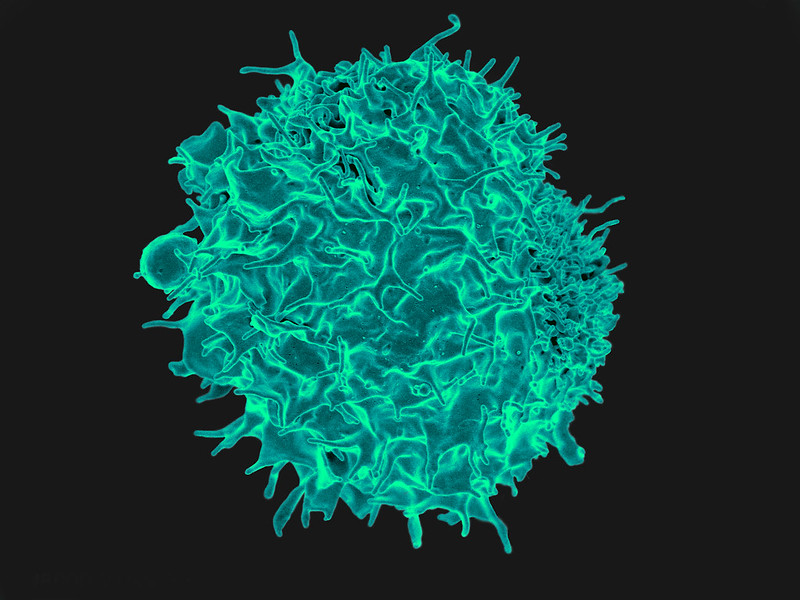
In November 2018, the media reported on a Chinese scientist who had created the world’s first gene-edited babies using CRISPR technology. He said his goal was to provide children with resistance to HIV, the virus that causes AIDS. When his experiment became public knowledge, twin girls had already been born and a third child was born the following year.
The fate of these three children, and whether they have experienced any negative long-term consequences from the embryonic genome editing, remains a closely guarded secret.
Controversial research
Considerable criticism followed the original birth announcement. Some argued that genetically modifying embryos to alter the traits of future children and generations should never be done.
Many pointed out that the rationale in this case was medically unconvincing – and indeed that safe reproductive procedures to avoid transmitting genetic diseases are already in widespread use, belying the justification typically given for heritable human genome editing. Others condemned his secretive approach, as well as the absence of any robust public consultation, considered a prerequisite for embarking on such a socially consequential path.
In the immediate aftermath of the 2018 revelation, the organizing committee of the Second International Summit on Human Genome Editing joined the global uproar with a statement condemning this research.
At the same time, however, the committee called for a “responsible translational pathway” toward clinical research. Safety thresholds and “additional criteria” would have to be met, including: “independent oversight, a compelling medical need, an absence of reasonable alternatives, a plan for long-term follow-up, and attention to societal effects.”
Notably, the additional criteria no longer included the earlier standard of “broad societal consensus.” https://www.youtube.com/embed/XAhFoaT6Kik?wmode=transparent&start=0 Nobel laureate David Baltimore, chair of the organizing committee for the Second International Summit on Human Genome Editing, talks about the importance of public global dialogue on gene editing.
New criteria
Now, it appears that South Africa has amended its Ethics in Health Research Guidelines to explicitly envisage research that would result in the birth of gene-edited babies.
Section 4.3.2 of the guidelines on “Heritable Human Genome Editing” includes a few brief and rather vague paragraphs enumerating the following criteria: (a) scientific and medical justification; (b) transparency and informed consent; (c) stringent ethical oversight; (d) ongoing ethical evaluation and adaptation; (e) safety and efficacy; (f) long-term monitoring; and (g) legal compliance.
While these criteria seem to be in line with those laid out in the 2018 summit statement, they are far less stringent than the frameworks put forth in subsequent reports. This includes, for example, the World Health Organization’s report Human Genome Editing: Framework for Governance (co-authored by Françoise Baylis).
Alignment with the law
Further, there is a significant problem with the seemingly permissive stance on heritable human genome editing entrenched in these research guidelines. The guidelines clearly require the research to comply with all laws governing heritable human genome research. Yet, the law and the research guidelines in South Africa are not aligned, which entails a significant inhibition on any possible research.
This is because of a stipulation in section 57(1) of the South African National Health Act 2004 on the “Prohibition of reproductive cloning of human beings.” This stipulates that a “person may not manipulate any genetic material, including genetic material of human gametes, zygotes, or embryos… for the purpose of the reproductive cloning of a human being.”
When this act came into force in 2004, it was not yet possible to genetically modify human embryos and so it’s not surprising there’s no specific reference to this technology. Yet the statutory language is clearly wide enough to encompass it. The objection to the manipulation of human genetic material is therefore clear, and imports a prohibition on heritable human genome editing.
Ethical concerns

The question that concerns us is: why are South Africa’s ethical guidelines on research apparently pushing the envelope with heritable human genome editing?
In 2020, we published alongside our colleagues a global review of policies on research involving heritable human genome editing. At the time, we identified policy documents — legislation, regulations, guidelines, codes and international treaties — prohibiting heritable genome editing in more than 70 countries. We found no policy documents that explicitly permitted heritable human genome editing.
It’s easy to understand why some of South Africa’s ethicists might be disposed to clear the way for somatic human genome editing research. Recently, an effective treatment for sickle cell disease has been developed using genome editing technology. Many children die of this disease before the age of five and somatic genome editing — which does not involve the genetic modification of embryos — promises a cure.
Implications on future research
But that’s not what this is about. So, what is the interest in forging a path for research on heritable human genome editing, which involves the genetic modification of embryos and has implications for subsequent generations? And why the seemingly quiet modification of the guidelines?
How many people in South Africa are aware that they’ve just become the only country in the world with research guidelines that envisage accommodating a highly contested technology? Has careful attention been given to the myriad potential harms associated with this use of CRISPR technology, including harms to women, prospective parents, children, society and the gene pool?
Is it plausible that scientists from other countries, who are interested in this area of research, are patiently waiting in the wings to see whether the law in South Africa prohibiting the manipulation of human genetic material will be an insufficient impediment to creating genetically modified children? Should the research guidelines be amended to accord with the 2004 statutory prohibition?
Or if, instead, the law is brought into line with the guidelines, would the result be a wave of scientific tourism with labs moving to South Africa to take advantage of permissive research guidelines and laws?
We hope the questions we ask are alarmist, as now is the time to ask and answer these questions.
Katie Hasson, Associate Director at the Center for Genetics and Society, co-authored this article.
Françoise Baylis, Distinguished Research Professor, Emerita, Dalhousie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.