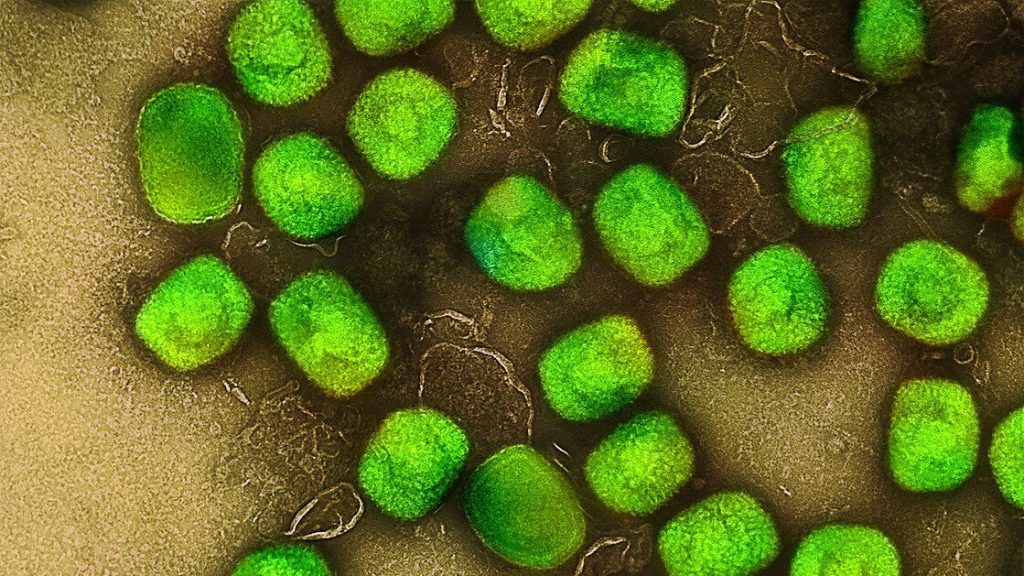
A team of researchers have found that the sunlight vulnerability of SARS-CoV-2 cannot be explained by the effect of UV-B rays alone.
Most of the COVID management concepts remain as true as in the first days of the pandemic, such as handwashing with soap and social distancing, though some have changed such as the notion of the virus mainly transmitted through droplets whereas evidence showed it can linger suspended in aerosol.
The researchers, from UC Santa Barbara, Oregon State University, University of Manchester and ETH Zurich. examined the well-known vulnerability of SARS-CoV-2 to sunlight. They concluded that exposure to UV-B radiation doesn’t completely account for its inactivation by sunlight.
The idea that an additional mechanism might be in play came when the team compared data from a July 2020 study that reported rapid sunlight inactivation of SARS-CoV-2 in a lab setting, with a theory of coronavirus inactivation by solar radiation that was published just a month earlier.
“The theory assumes that inactivation works by having UV-B hit the RNA of the virus, damaging it,” said lead author Paolo Luzzatto-Fegiz, UC Santa Barbara mechanical engineering professor. “Judging from the discrepancies between the experimental results and the predictions of the theoretical model, however, the research team felt that RNA inactivation by UV-B “might not be the whole story.”
Experimentation showed 10-20 minutes to reach virus inactivation—much faster than the theory’s predictions. Viruses in simulated saliva were inactivated over eight times faster when irradiated by UV-B lamps than would have been predicted by the theory, while those cultured in a complete growth medium before exposure to UV-B were inactivated over three times faster. In order to match theory, SARS-CoV-2 would then have greater UV-B sensitivity than any currently known virus.
“The theory predicts that inactivation should happen an order of magnitude slower,” Prof Luzzatto-Fegiz said.
There might be another mechanism involved besides UV-B effects on RNA; such as the synergistic effect of the less energetic UV-A rays.
“People think of UV-A as not having much of an effect, but it might be interacting with some of the molecules in the medium,” he said. Such reactive intermediate molecules could be hastening virus inactivation, a concept known in wastewater treatment and other environmental science fields.
“So, scientists don’t yet know what’s going on,” Luzzatto-Fegiz said. “Our analysis points to the need for additional experiments to separately test the effects of specific light wavelengths and medium composition.”
These findings could help develop ways to control the virus with widely available UV-A and UV-B sources. Sources which emit UV-C, which is otherwise blocked by the atmosphere, has proven effective in certain settings such as air filtration but its high energy limits applications and raises safety concerns.
“UV-C is great for hospitals,” said co-author Julie McMurry. “But in other environments—for instance kitchens or subways—UV-C would interact with the particulates to produce harmful ozone.”
Co-author and UCSB mechanical engineering professor Yangying Zhu added that UV-A’s possible effectiveness meant that inexpensive UV-A LEDs many times brighter than UV-A in normal sunlight could be used. UV-A could be used more for air filtration for example, but the specifics of each setting warrant consideration, said co-author Fernando Temprano-Coleto.
Source: Medical Xpress
Journal information: Paolo Luzzatto-Fegiz et al. UVB Radiation Alone May Not Explain Sunlight Inactivation of SARS-CoV-2, The Journal of Infectious Diseases (2021). DOI: 10.1093/infdis/jiab070