More Monkeypox Antibodies with Childhood Smallpox Vaccination
In a study published in Cell Host & Microbe, scientists studied the sensitivity of MPXV, the virus that causes mpox (formerly monkeypox) to neutralising antibodies (NAbs) generated after infection with the virus and/or vaccination with IMVANEX. They found that those who had been born before 1980 had more antibodies in response to either IMVANEX vaccination or mpox infection, highlighting the lasting protection of smallpox vaccination.
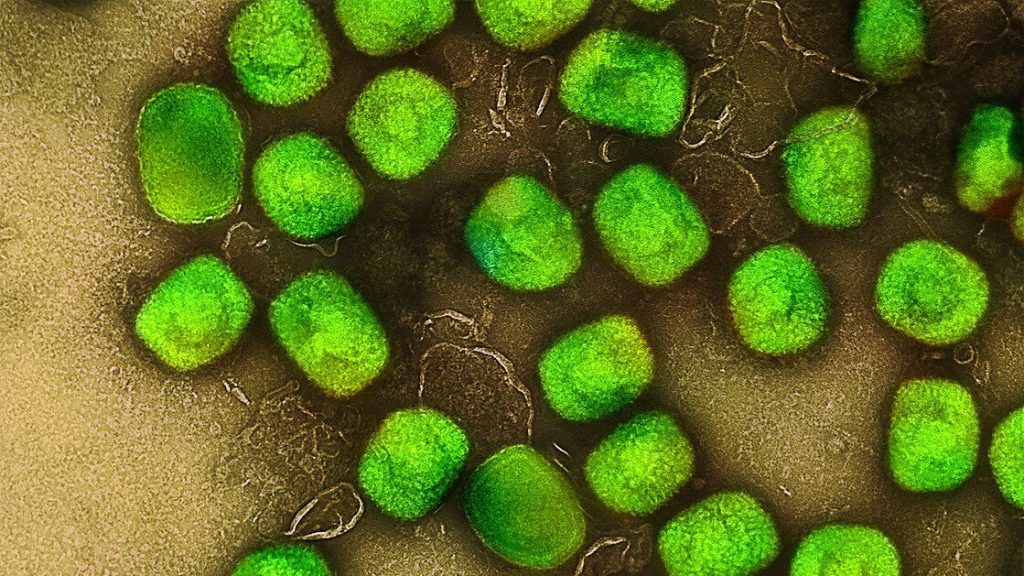
The IMVANEX vaccine has been used as pre- and post-exposure prophylaxis in high-risk populations, but its effectiveness is not yet well characterised. To analyse the sensitivity of the virus, a team of scientists led by Pasteur Institut developed two cellular tests to quantify neutralising antibodies, using either the attenuated virus as a vaccine (MVA) or an MPXV strain isolated in a recently infected individual.
In 2022-2023, an unprecedented epidemic of 87 000 cases of mpox occurred in non-endemic areas, affecting people with no direct link to travel in Central or West Africa, where the virus has historically been present. MPXV is mainly transmitted to humans by rodents, with human-to-human transmission occurring via respiratory droplets or close contact. Symptoms are less severe than those of smallpox, and the case-fatality rate is lower. MPXV is still circulating at very low levels in non-endemic areas, which is why it is important to improve characterisation and analyse the immune response of people infected with the virus or vaccinated with IMVANEX, the third-generation vaccine currently available, initially developed for smallpox.
The large number of sera analysed provided good statistical power, meaning that the analysis could be narrowed to subgroups of patients based on various criteria such as age.
The study demonstrated the role of complement, already known for other poxviruses, and the neutralising activity of the antibodies generated by infection or vaccination. Robust levels of anti-MVA antibodies were detected after infection, vaccination with the historic smallpox vaccine, or administration of IMVANEX or another MVA-based vaccine candidate. MPXV was minimally sensitive to neutralisation in the absence of complement. The addition of complement from sera enhanced detection of individuals with antibodies and increased their level of anti-MPXV antibodies. Four weeks after infection, anti-MVA and -MPXV NAbs were observed in 94% and 82% of individuals, respectively. Two doses of IMVANEX generated anti-MVA and -MPXV NAbs that were detectable in 92% and 56% of vaccinees, respectively.
The highest level of antibodies was found in individuals born before 1980 (who had therefore been vaccinated for smallpox), whether after infection or after administration of IMVANEX, highlighting the impact of historic smallpox vaccination on immune responses to infection or administration of IMVANEX. This suggests that a sort of hybrid immunity was generated in infected individuals who were vaccinated in childhood.
The number of MPXV infections has been constantly on the rise since mass vaccination for smallpox was discontinued in the 1980s. “The neutralisation assays developed in connection with this research may help define correlates of protection against infection or disease severity. The assays can also be used to conduct epidemiological surveys, assess the duration of protection conferred by previous infection or by authorised and candidate vaccines, and analyse the use of immunotherapeutic intervention. The assays represent useful tools to understand the mechanisms of multiplication of MPXV and its effects on public health, and to optimsze patient treatment,” commented Olivier Schwartz, Head of the Institut Pasteur’s Virus and Immunity Unit and last author of the study.
Source: Institut Pasteur





