New Viral Treatment for Basal Cell Carcinoma Shines in Trials

Basal cell carcinomas, the most common form of skin cancer, occur in chronically sun-exposed areas such as the face. Locally advanced tumours in particular can be difficult to treat surgically. A research team from MedUni Vienna and University Hospital Vienna has now investigated the effectiveness of a new type of therapy and achieved promising results: The active substance TVEC led to a reduction in the size of the basal cell carcinoma in all study participants, which not only improved surgical removal, but also led to a complete regression of the tumour in some of the patients. The study was published in the top journal Nature Cancer.
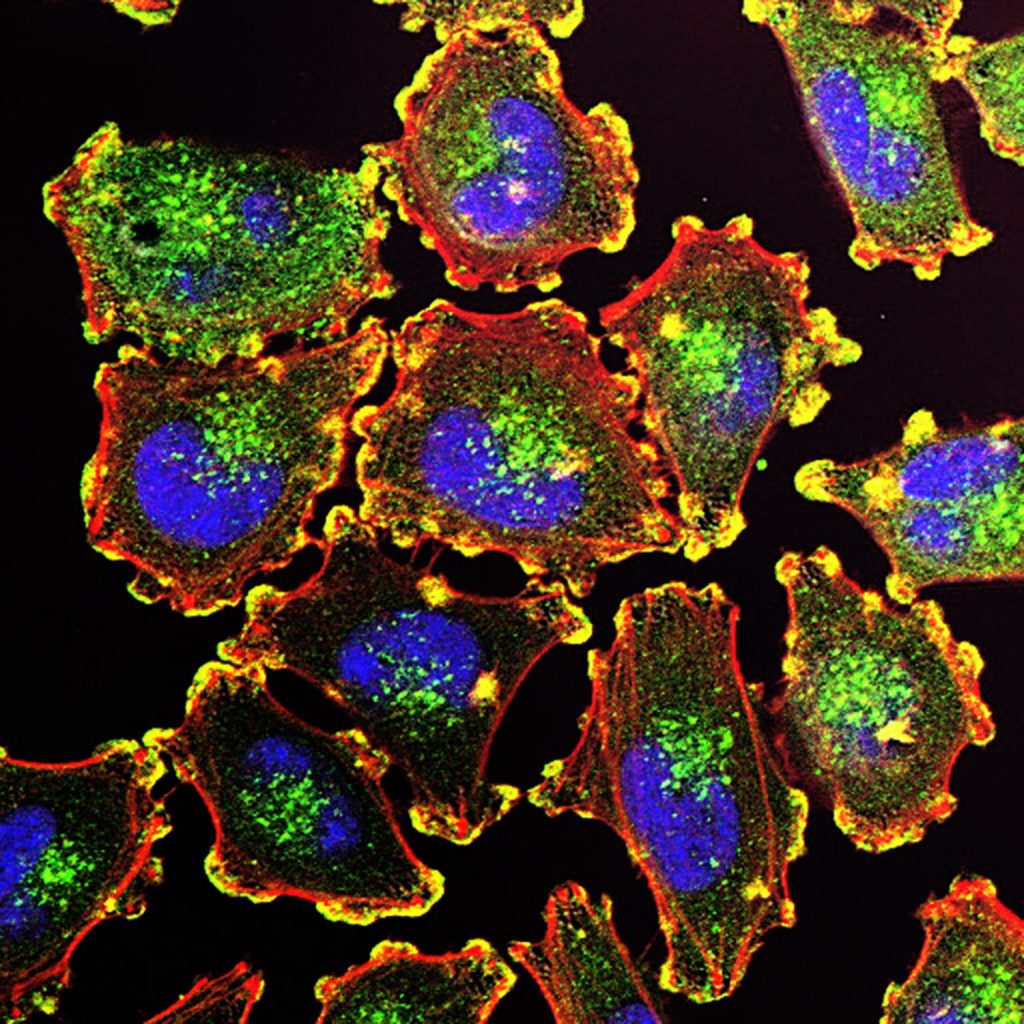
In the study Talimogene Laherparepvec (TVEC) was used, which has so far only been approved for the treatment of superficial melanoma metastases. TVEC is a genetically modified herpes simplex virus that specifically destroys tumour cells and simultaneously activates the immune system. The aim of the study was to reduce the size of the tumour before a planned operation so that patients would not suffer any functional or cosmetic restrictions after the procedure. The study included 18 patients who would have required a flap or skin graft due to the size and localisation of their basal cell carcinoma. They each received six intralesional injections of TVEC over a period of 13 weeks before the tumour was surgically removed.
“This enabled the tumour to be reduced in size in half of the patients to such an extent that surgery with direct wound closure was possible. In a third of the cases, the subsequent histological examination even showed no more living tumour cells. All treated tumours at least became smaller, and no tumour grew further under the therapy. The treatment was well tolerated by the patients,” says the principal investigator Christoph Höller, Head of the Skin Tumour Centre at the Department of Dermatology, summarising the results. “The new treatment option for basal cell carcinoma can not only simplify surgery, but also help to avoid disfiguring operations and functional limitations,” adds first author Julia Ressler, also from the Department of Dermatology. In addition to the clinical studies, the researchers from the Department of Dermatology, in cooperation with the St. Anna Children’s Hospital, carried out comprehensive analyses that show that the immune defence in the tumour tissue is strengthened in the course of therapy with TVEC.
These results suggest that TVEC could be a promising option for the neoadjuvant, i.e. pre-surgical, treatment of basal cell carcinoma, particularly in patients for whom major surgery should be avoided. Further studies are to follow in order to confirm the benefits of this new option in a larger patient population.
Source: Medical University of Vienna