Why Antibiotics can Fail Even against Non-resistant Bacteria

Antibiotics are indispensable for treating bacterial infections. But why are they sometimes ineffective, even when the bacteria are not resistant? In their latest study published in the journal Nature, researchers from the University of Basel challenge the conventional view that a small subset of particularly resilient bacteria are responsible for the failure of antibiotic therapies.
In certain infectious diseases caused by bacteria, antibiotics are less effective than expected. One example is infections caused by Salmonella bacteria, which can lead to illnesses such as typhoid fever. For many years, researchers believed that a small subset of dormant bacteria are the main problem in fighting infections. These so-called persisters can survive antibiotic treatment and cause relapses later. Researchers worldwide have been working on new therapies aimed at targeting and eliminating these “sleeping” bacteria.
In a new study, Professor Dirk Bumann’s team from the Biozentrum of the University of Basel challenges the prevailing concept that persisters are the cause of antibiotic ineffectiveness. “Contrary to widespread belief, antibiotic failure is not caused by a small subset of persisters. In fact, the majority of Salmonella in infected tissues are difficult to kill,” explains Bumann. “We have been able to demonstrate that standard laboratory tests of antimicrobial clearance produce misleading results, giving a false impression of a small group of particularly resilient persisters.”
Nutrient starvation increases Salmonella resilience
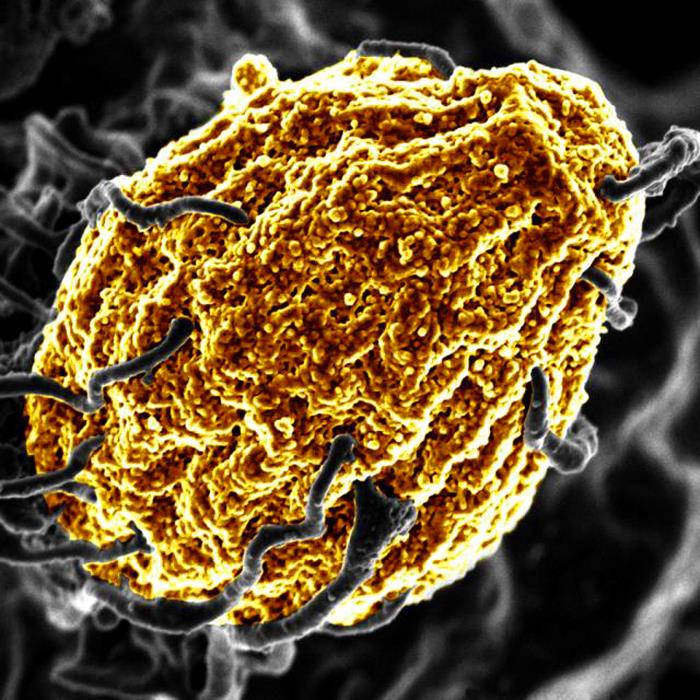
The researchers investigated antimicrobial clearance in both Salmonella-infected mice and tissue-mimicking laboratory models. The body’s defense mechanisms against bacteria often include reducing the availability of nutrients. The researchers have now revealed that in fact, this nutrient starvation is the main reason for Salmonella bacteria surviving treatments with antibiotics. The researchers assume that the same applies to other bacterial pathogens.
“Under nutrient-scarce conditions, bacteria grow very slowly,” says Bumann. “This may seem good at first, but is actually a problem because most antibiotics only gradually kill slowly growing bacteria.” As a result, the drugs are much less effective, and relapses can occur even after prolonged therapy.
Real-time analyses reveal misconception
The scientists used an innovative method to monitor antibiotic action in single bacteria in real time. “We demonstrated that nearly the entire Salmonella population survives antibiotic treatment for extended periods, not just a small subset of hyper-resilient persisters,” says first author Dr Joseph Fanous.
A major issue with the standard methods used worldwide for decades is their indirect and delayed measurement of bacterial survival, leading to distorted results. “Traditional tests underestimate the number of surviving bacteria,” explains Fanous. “And they falsely suggest the presence of hyper-resilient subsets of persisters that do not actually exist.” This misinterpretation has influenced research for many years.
Novel tools for antibiotics research
These findings could fundamentally change antibiotics research. “Our work underlines the importance of studying bacterial behaviour and antibiotic effects live and under physiologically relevant conditions,” emphasises Bumann. “In a few years, modern methods like real-time single-cell analysis will hopefully become standard.” Shifting the focus from persisters to the impact of nutrient starvation is an important step toward more effective therapies against difficult-to-treat infections.
The project is part of the National Center of Competence in Research (NCCR) “AntiResist”. The research consortium aims to develop innovative strategies to combat bacterial infections. Dirk Bumann is one of the directors of the NCCR “AntiResist”.
Source: University of Basel