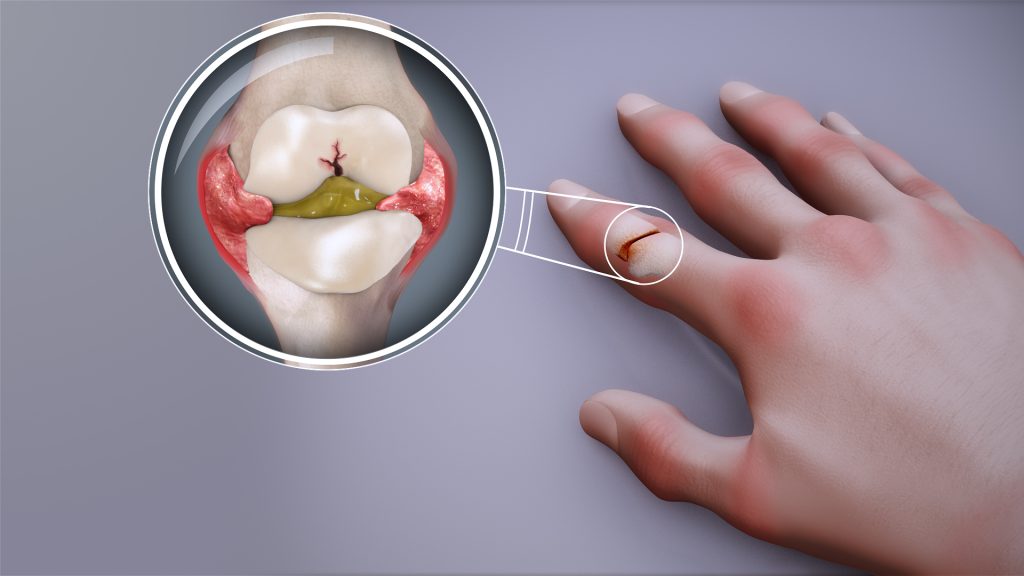
Muscle Wasting Reversed in Patients with Rheumatoid Arthritis

Patients with rheumatoid arthritis increased their leg muscle volume when treated with an anti-rheumatic drug, offering new hope for improved muscle health.
Publishing in the prestigious journal, The Lancet Rheumatology, a team from Newcastle University and The Newcastle upon Tyne Hospitals NHS Foundation Trust describe how 15 patients were given Tofacitinib, a Janus kinase (JAK) inhibitor used to treat RA, as part of an experimental medicine study. After six months, their leg muscles increased in size, particularly in the thigh.
Sarcopenia is a progressive, age-related musculoskeletal disease characterized by the loss of muscle mass, strength, and physical performance, increasing the risk of falls, fractures, physical disability, and mortality. Currently there are no medicines approved to reverse this muscle-wasting disease. It is commonly seen in patients with rheumatoid arthritis where chronic inflammation contributes to the loss of muscle mass and strength.
The Rheumatoid Arthritis and MUScle (RAMUS) study
In this study, the leg muscles of 15 patients were measured by MRI scans at one month and at six months. After 6 months, participants’ muscle volume had increased by 4% for the whole leg, equating to an average increase of 242 cm3, and by 5% for the thigh.
Alongside the increase in muscle volume, the RAMUS study also reported changes in the gene expression in muscle tissue with treatment, which were opposite to changes seen in ageing muscle.
Dr Joshua Bennett, NIHR Clinical Lecturer at Newcastle University and Paediatric Rheumatology Registrar within the Newcastle Upon Tyne Hospitals NHS Trust and lead author of the paper said: “This small study is the first to show that JAK inhibitor drugs may be able to reverse sarcopenia in rheumatoid arthritis. We know that sarcopenia is also seen in many other diseases and in old age, but no drugs have been approved to reverse it. Larger studies are now needed to test our findings, but it is exciting to think of the potential for these drugs to treat muscle wasting.”
13 patients experienced adverse events, the majority of which were mild. The team say a larger, follow up study is needed which would include a control group.
Supports growing evidence
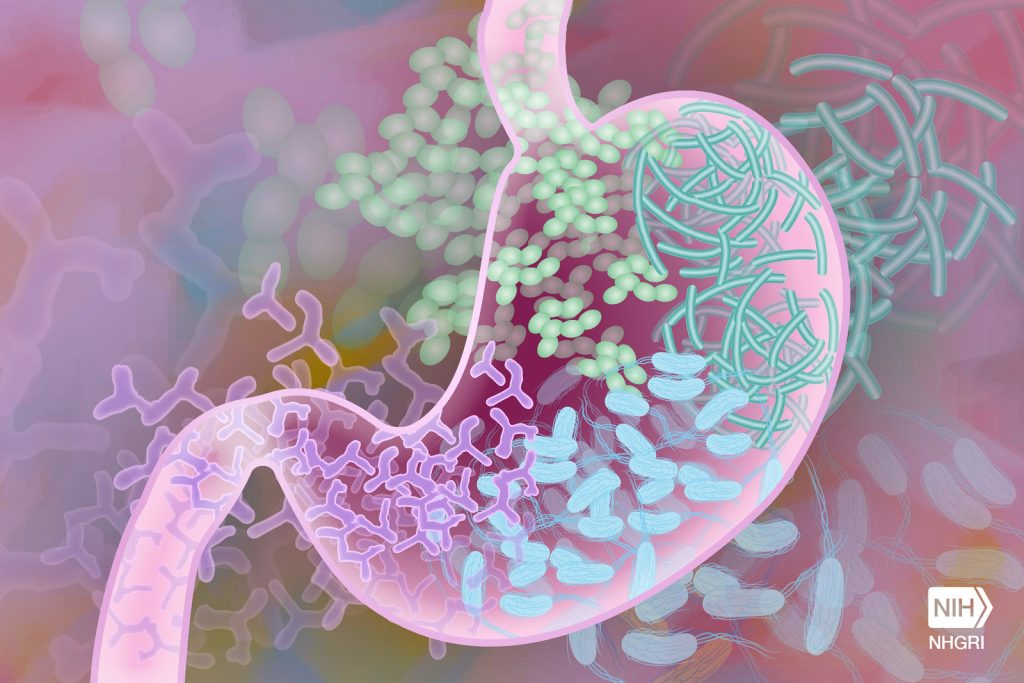
Professor John Isaacs, Professor of Clinical Rheumatology, Newcastle University, Director of Research at Newcastle Hospitals and Deputy Director of the National Institute for Health and Care Research (NIHR) Newcastle Biomedical Research Centre (BRC) who led the study added: “Our findings support growing evidence that inflammation, as evidenced by pro-inflammatory cytokines, may contribute to muscle loss.
“Tofacitinib treatment led to increased muscle volume in patients and triggered changes in muscle gene activity that run counter to the patterns typically seen in age-related muscle decline, suggesting a distinct biological effect.
“While this research did not demonstrate improved muscle strength, patients with arthritis often struggle to perform strength tests due to joint pain and so this does not diminish the potential benefits of reversing sarcopenia as we know it increases the risk of falls, fractures, physical disability, and mortality.”
The primary study funding was by Pfizer, with The BMA Foundation, the JGW Patterson Foundation and the Newcastle Hospitals Charity also contributing. RAMUS was also supported by the NIHR Newcastle Biomedical Research Centre (BRC) and Clinical Research Facility.
Source: Newcastle University