A Simple Technique to Reduce Light-headedness upon Standing Up
Light-headedness upon standing up due to initial orthostatic hypotension (IOH) is a common but poorly understood condition. A new study offers two simple techniques to effectively manage symptoms of IOH and improve quality of life by activating lower body muscle before or after standing. The research appears in Heart Rhythm.
IOH is a transient decrease in blood pressure and increase in heart rate. Syncope, light-headedness, dizziness, or loss of consciousness from IOH, affects up to 40% of the general population (all ages), while presyncope is probably even more common. However, the condition is under-studied and there are very few options currently available to patients with IOH and no pharmacological treatments. The most common recommendations have been to stand up slowly or sit up first before standing.
IOH symptoms often present during an active stand but not with a passive tilt-table test, suggesting that a muscle activation response plays an important role in the pathophysiology of IOH. This muscle activation response refers to the rapid and excessive vasodilation that occurs in response to the brief lower body muscle contraction required to stand due to local mechanisms. Additional factors involved in this response include the increase in heart rate, initially due to the muscle heart reflex and secondarily in response to the arterial baroreflex triggered by the drop in BP as well as the increase in peripheral resistance, which is also triggered by the arterial baroreflex.
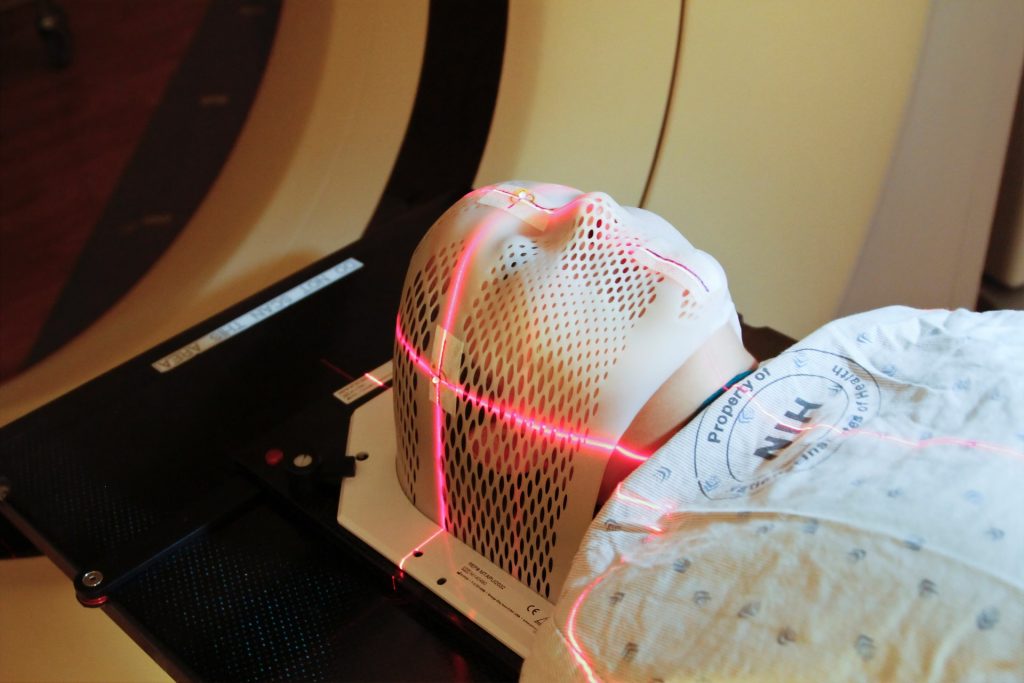
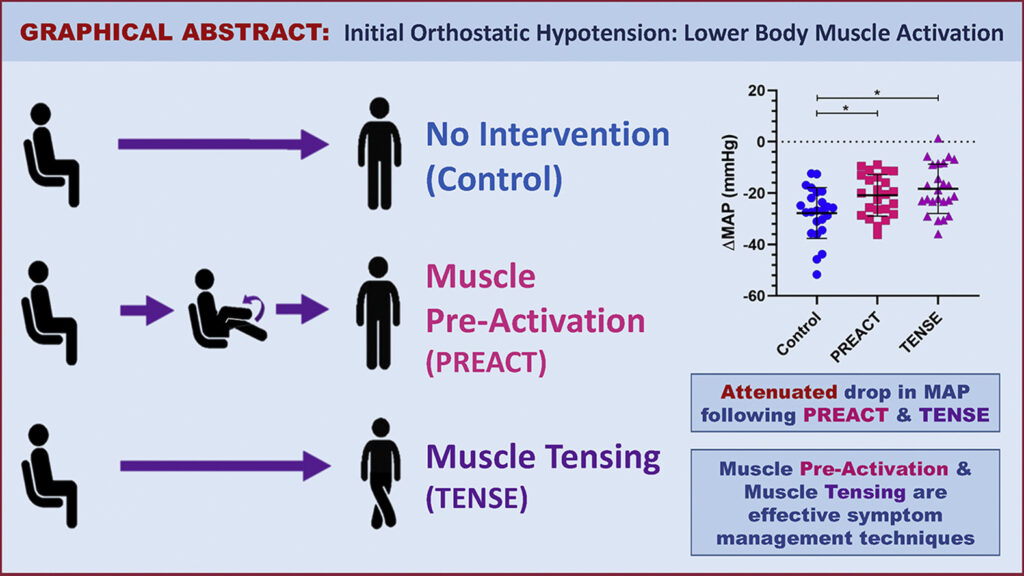
This study investigated physical manoeuvres before or after standing and their efficacy in reducing the drop in blood pressure as well as the symptoms typically seen in IOH patients upon standing. Study participants included 24 young women with a history of IOH. Two participants had inadequate heart rate recordings and were excluded from the analysis. The interventions tested consisted of lower body muscle pre-activation (thighs) through repeated knee raises prior to standing (PREACT) and lower body muscle tensing (thighs and buttocks) through leg crossing and tensing immediately after standing (TENSE).
The 22 study participants completed three sit-to-stand manoeuvres including a stand with no intervention (control), and two interventions. Researchers found that both PREACT and TENSE effectively improve the blood pressure drop. This led to a reduction in symptoms upon standing. They found that the PREACT manoeuvre accomplished this by increasing cardiac output, while the TENSE manoeuvre did so by increasing stroke volume.
“Our study provides a novel and cost-free symptom management technique that patients with IOH can use to manage their symptoms,” noted first author Nasia A. Sheikh, MSc. “Since it is a physical manoeuvre, it simply requires the lower body limbs, which patients can utilise at any time and from anywhere to combat their symptoms.”
Source: Elsevier