Plant-rich, Low Saturated-fat Diet Linked to Reduced Psoriasis Severity

A new study by researchers at King’s College London, published in the British Journal of Nutrition, has found significant associations between diet quality and the severity of psoriasis. The findings provide novel insights into how dietary patterns may be related to psoriasis severity in non-Mediterranean populations.
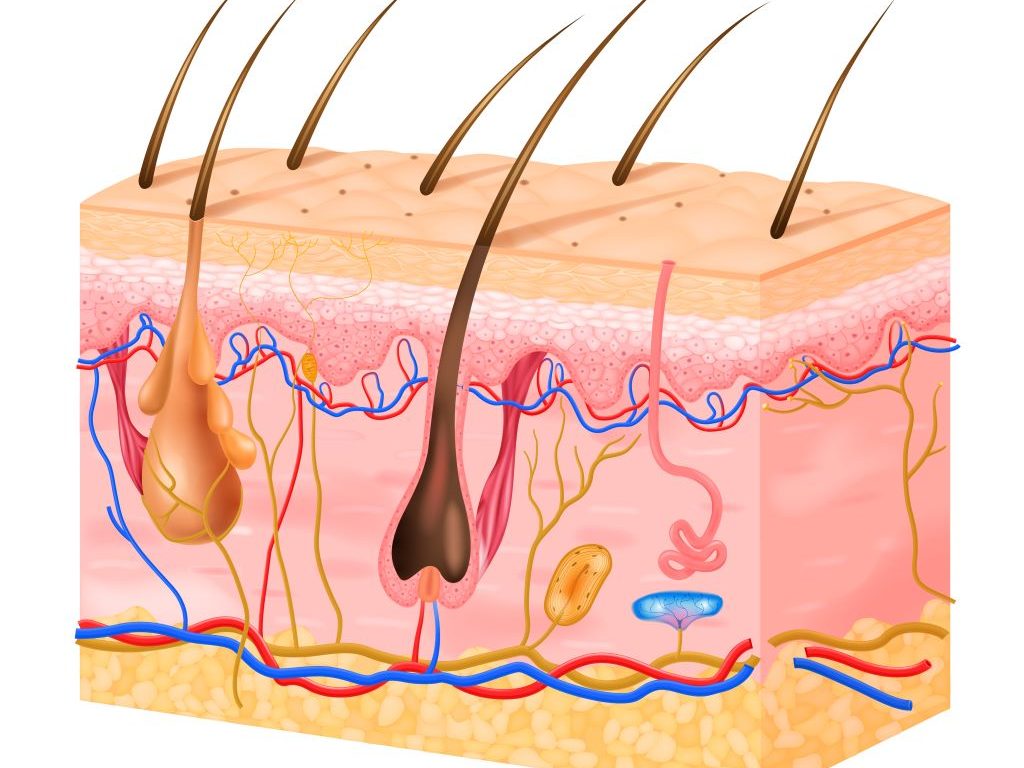
Psoriasis is a long-lasting inflammatory skin disease which causes flaky patches of skin that form scales. It affects millions worldwide and is believed to be caused by a problem with the immune system.
The research analysed data from 257 adults with psoriasis who had completed an online survey. Participants’ adherence to various diet quality scores, including the Mediterranean Diet Score, the Dietary Approaches to Stop Hypertension (DASH) score, and the Healthy Plant-based Diet Index, was assessed using a food frequency questionnaire. Psoriasis severity was self-assessed using a validated questionnaire.
Key findings from the study indicate that individuals with very low adherence to the DASH diet index and the Healthy Plant-based Diet Index were significantly more likely to report higher psoriasis severity.
Further analysis of the different elements of the DASH dietary pattern revealed that greater red and processed meat intake was associated with more severe psoriasis even when body mass index (BMI) was considered. Fruits, nuts and legume intakes were also associated with less severe psoriasis, but this relationship was not independent of BMI.
The study was published as part of the Asking People with Psoriasis about Lifestyle and Eating (APPLE) project and funded by the Psoriasis Association.
Our findings point to the potential benefits of dietary interventions in improving patient outcomes. Given the impact of psoriasis on physical and psychological well-being, incorporating dietary assessments into routine care could offer patients additional support in managing their condition.
Sylvia Zanesco, PhD student from the Department of Nutritional Sciences at King’s College London who led the research
The DASH dietary pattern was originally designed to lower blood pressure and emphasises fruits, vegetables, whole grains, low-fat dairy foods and lean meats while limiting salt, sugar, and saturated fats. A high Healthy Plant-based Diet Index characterises a dietary pattern rich in healthy plant foods including fruits and vegetables, whole grains, nuts and seeds, legumes and plant oils rich in unsaturated fats, as well as being low in animal foods and unhealthy plant foods such as sugary foods and drinks and refined starches.
The study accounted for several confounding factors, including age, sex, smoking status, alcohol, energy intake, and mental health, ensuring a comprehensive analysis of dietary patterns that are independently associated with psoriasis severity.
This research brings much-needed evidence that there may be a role for dietary advice, alongside standard clinical care, in managing symptoms of psoriasis. Our next steps will be to explore whether diets rich in healthy plant foods can reduce symptoms of psoriasis in a controlled clinical trial.
Professor Wendy Hall, Professor of Nutritional Sciences at King’s College London and senior author of the study
The findings of the study contribute to the growing body of evidence supporting dietary modification as a complementary strategy in psoriasis management to potentially alleviate disease severity and improve patients’ quality of life.
Source: King’s College London