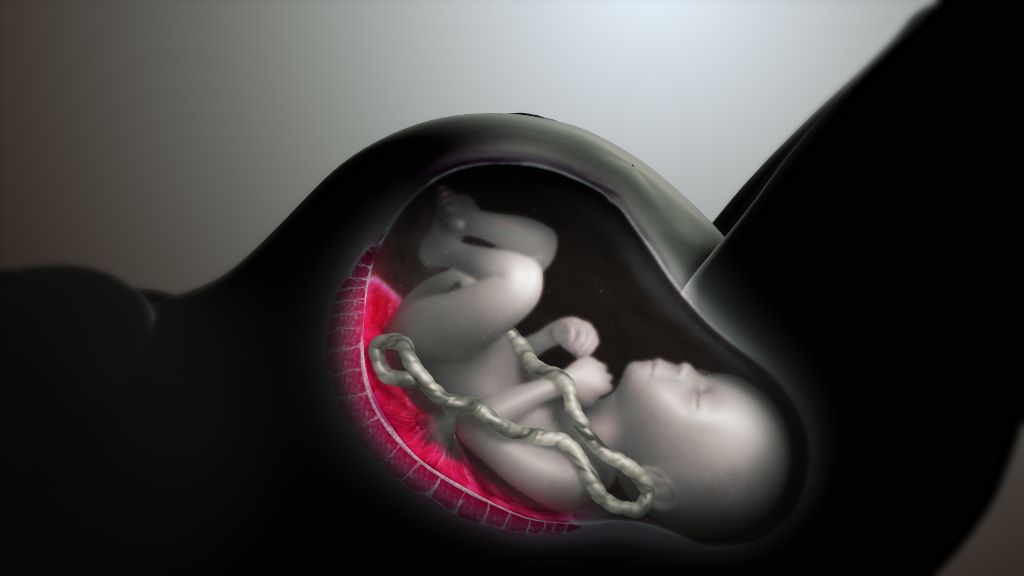
Microplastics Found in Every Human Placenta Tested in Study
A flurry of recent studies has found that microplastics are present in virtually everything we consume, from bottled water to meat and plant-based food. Now, University of New Mexico Health Sciences researchers have used a new analytical tool to measure the microplastics present in human placentas.
In a study published in the journal Toxicological Sciences, a team led by Matthew Campen, PhD, Regents’ Professor in the UNM Department of Pharmaceutical Sciences, reported finding microplastics in all 62 of the placenta samples tested, with concentrations ranging from 6.5 to 790 micrograms per gram of tissue.
Although those numbers may seem small, Campen is worried about the health effects of a steadily rising volume of microplastics in the environment.
For toxicologists, “dose makes the poison,” he said. “If the dose keeps going up, we start to worry. If we’re seeing effects on placentas, then all mammalian life on this plant could be impacted. That’s not good.”
In the study, Campen and his team, partnering with colleagues at the Baylor College of Medicine and Oklahoma State University, analyzed donated placenta tissue. In a process called saponification, they chemically treated the samples to “digest” the fat and proteins into a kind of soap.
Then, they spun each sample in an ultracentrifuge, which left a small nugget of plastic at the bottom of a tube. Next, using a technique called pyrolysis, they put the plastic pellet in a metal cup and heated it to 600 degrees Celsius, then captured gas emissions as different types of plastic combusted at specific temperatures.
“The gas emission goes into a mass spectrometer and gives you a specific fingerprint,” Campen said. “It’s really cool.”
The researchers found the most prevalent polymer in placental tissue was polyethylene, which is used to make plastic bags and bottles. It accounted for 54% of the total plastics. Polyvinyl chloride (better known as PVC) and nylon each represented about 10% of the total, with the remainder consisting of nine other polymers.
Marcus Garcia, PharmD, a postdoctoral fellow in Campen’s lab who performed many of the experiments, said that until now, it has been difficult to quantify how much microplastic was present in human tissue. Typically, researchers would simply count the number of particles visible under a microscope, even though some particles are too small to be seen.
With the new analytical method, he said, “We can take it to that next step to be able to adequately quantify it and say, ‘This is how many micrograms or milligrams,’ depending on the plastics that we have.”
Plastic use worldwide has grown exponentially since the early 1950s, producing a metric ton of plastic waste for every person on the planet. About a third of the plastic that has been produced is still in use, but most of the rest has been discarded or sent to landfills, where it starts to break down from exposure to ultraviolet radiation present in sunlight.
“That ends up in groundwater, and sometimes it aerosolizes and ends up in our environment,” Garcia said. “We’re not only getting it from ingestion but also through inhalation as well. It not only affects us as humans, but all off our animals — chickens, livestock — and all of our plants. We’re seeing it in everything.”
Campen points out that many plastics have a long half-life — the amount of time needed for half of a sample to degrade. “So, the half-life of some things is 300 years and the half-life of others is 50 years, but between now and 300 years some of that plastic gets degraded,” he said. “Those microplastics that we’re seeing in the environment are probably 40 or 50 years old.”
While microplastics are already present in our bodies, it is unclear what health effects they might have, if any. Traditionally, plastics have been assumed to be biologically inert, but some microplastics are nanometres in size and are capable of crossing cell membranes, he said.
Campen said the growing concentration of microplastics in human tissue might explain puzzling increases in some types of health problems, such as inflammatory bowel disease and colon cancer in people under 50, as well as declining sperm counts.
The concentration of microplastics in placentas is particularly troubling, he said, because the tissue has only been growing for eight months (it starts to form about a month into a pregnancy). “Other organs of your body are accumulating over much longer periods of time.”
Campen and his colleagues are planning further research to answer some of these questions, but in the meantime he is deeply concerned by the growing production of plastics worldwide.
“It’s only getting worse, and the trajectory is it will double every 10 to 15 years,” he said. “So, even if we were to stop it today, in 2050 there will be three times as much plastic in the background as there is now. And we’re not going to stop it today.”



