US, Europe Report Severe Hepatitis of Unknown Aetiology in Children

Public health officials are puzzling over cases of severe hepatitis in children reported in Europe and the US. A number of the cases have tested positive for adenovirus and/or SARS-CoV-2, though what role these viruses play is not yet clear.
On 5 April 2022, UK authorities notified the World Health Organization was of 10 cases of severe acute hepatitis of unknown aetiology in previously healthy young children ranging in from 11 months to five years old across central Scotland. Nine had onset of symptoms in March 2022, and all cases were detected on hospitalisation. Symptoms included jaundice, diarrhoea, vomiting and abdominal pain. An article published in Eurosurveillance detailed the cases.
Further investigations across the UK identified a total of 74 cases as of 8 April (including the 10 cases) that fulfilled the case definition. The clinical syndrome in identified cases is of acute hepatitis with markedly elevated liver enzymes, often with jaundice, sometimes preceded by gastrointestinal symptoms, in children principally up to 10 years old. Some cases have required transfer to specialist children’s liver units and six children have undergone liver transplantation. As of 11 April, no death has been reported among these cases and one epidemiologically linked case has been detected.
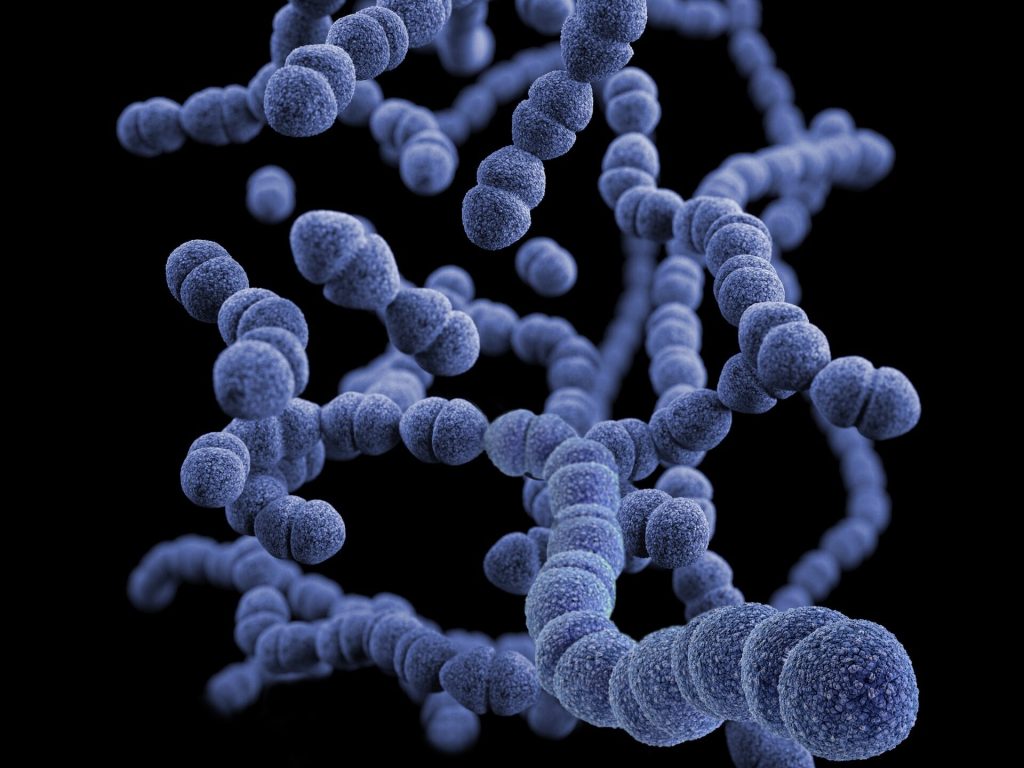
Laboratory testing has excluded hepatitis type A, B, C, and E viruses (and D where applicable) in these cases while SARS-CoV-2 and/or adenovirus have been detected in several cases. The United Kingdom has recently observed an increase in adenovirus activity, which is co-circulating with SARS-CoV-2, though the role of these viruses in the pathogenesis is not yet clear. They have however been linked to bladder inflammation and infection, and on occasion to hepatitis, but it is rare in children who are not immunocompromised.
To date, no other epidemiological risk factors have been identified, including recent international travel. Overall, the aetiology of the current hepatitis cases is still considered unknown and remains under active investigation. Laboratory testing for additional infections, chemicals and toxins is underway for the identified cases.
Following the notification from the UK, less than five cases (confirmed or possible) have been reported in Ireland, further investigations into these are ongoing. Additionally, three confirmed cases of acute hepatitis of unknown aetiology have been reported in children (ranging in age from 22 months-old to 13 years old) in Spain. A further 9 have been reported in the US state of Alabama, with five testing positive for adenovirus.
Karen Landers, district medical officer for the Alabama Department of Public Health, said that the cases were spread across the state, and no links were found among the children.
“It is not common to see children with severe hepatitis,” Landers told STAT in an interview. “Seeing children with severe [hepatitis] in the absence of severe underlying health problems is very rare. That’s what really stood out to us in the state of Alabama.”
Source: WHO