Hair Loss Tied to High-fat Diets or Genetic Obesity

A mouse study by Japanese researchers found that high-fat diets or genetically induced obesity can cause loss of hair follicles.
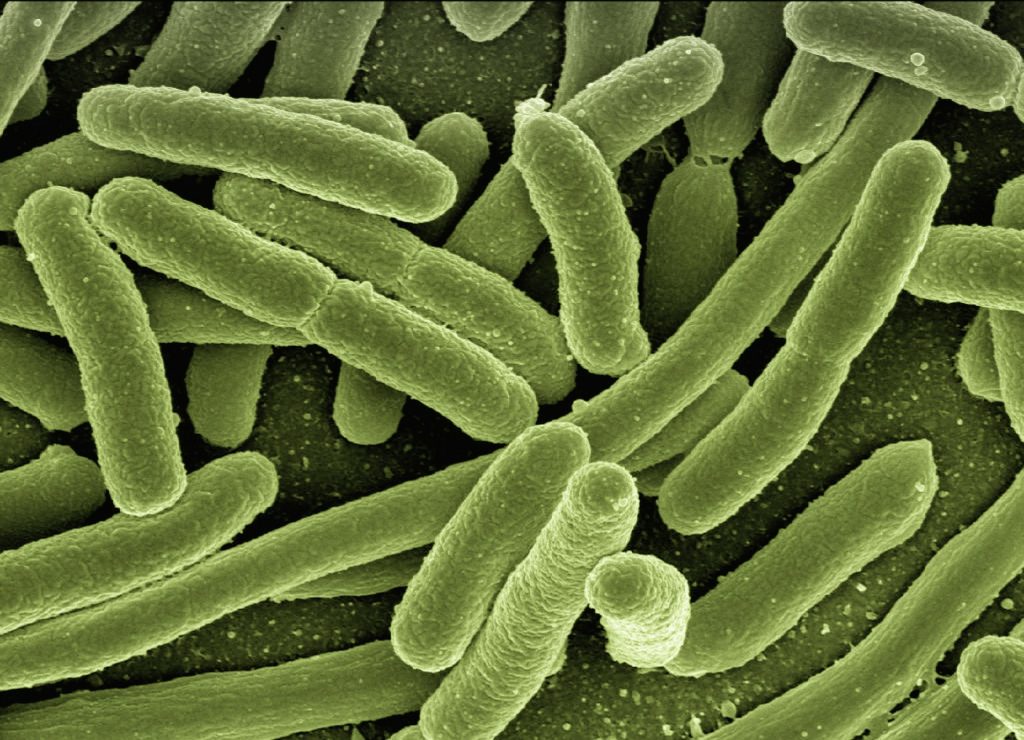
Obesity is linked to the development of numerous diseases in humans, such as heart disease and diabetes. However, it’s not fully clear how body organs specifically deteriorate and lose functionality from chronic obesity. Using mice, researchers from Tokyo Medical and Dental University (TMDU) examined how a high-fat diet or genetically induced obesity can affect hair thinning and loss. The findings, published in Nature, indicated that obesity can lead to depletion of hair follicle stem cells (HFSCs) by inducing certain inflammatory signals, blocking hair follicle regeneration and ultimately resulting in loss of hair follicles.
HFSCs normally renew themselves every hair follicle cycle. With progressing age, HFSCs fail to renew themselves leading to fewer HFSCs and therefore hair thinning. Although overweight people have a higher risk of male pattern balding, whether obesity accelerates hair thinning, how it does this and the molecular mechanisms behind it have remained largely a mystery. The TMDU group aimed to address those questions and identified some of the mechanisms.
Explaining the study, study lead author Hironobu Morinaga said: “High-fat diet feeding accelerates hair thinning by depleting HFSCs that replenish mature cells that grow hair, especially in old mice. We compared the gene expression in HFSCs between HFD-fed mice and standard diet-fed mice and traced the fate of those HFSCs after their activation.
“We found that those HFSCs in HFD-fed obesed mice change their fate into the skin surface corneocytes or sebocytes that secrete sebum upon their activation. Those mice show faster hair loss and smaller hair follicles along with depletion of HFSCs.
“Even with HFD feeding in four consecutive days, HFSCs show increased oxidative stress and the signs of epidermal differentiation.”
“The gene expression in HFSCs from the high-fat–fed mice indicated the activation of inflammatory cytokine signaling within HFSCs,” said senior author Emi Nishimura. “The inflammatory signals in HFSCs strikingly repress the Sonic hedgehog signaling that plays a crucial role in hair follicle regeneration in HFSCs.
However, the researchers noted that activating the Sonic hedgehog signaling pathway in this process can rescue the depletion of HFSCs. “This could prevent the hair loss brought on by the high-fat diet,” said Nishimura.
This study shines a light on cellular and tissue dysfunction from a high-fat diet or genetically induced obesity, and could lead to prevention and treatment of hair thinning along with greater understanding of obesity-related diseases.