Significant Gaps between Obesity Science and Patient Care

As research continues to produce evidence about the underlying causes of obesity and optimal strategies to treat and manage obesity have evolved, there are disparities in application of the latest scientific advances in the clinical care for people with obesity. Widespread adoption of current findings, consistency of care and expertise in obesity care varies by health care professional and institution. These findings are detailed in a new American Heart Association scientific statement, “Implementation of Obesity Science Into Clinical Practice,” published in the journal Circulation.
“Obesity is undeniably a critical public health concern in the U.S. and around the world, affecting nearly all populations and straining our health care systems,” said Deepika Laddu, Ph.D., FAHA, chair of the statement writing committee and a senior research scientist at Arbor Research Collaborative for Health in Ann Arbor, Michigan. “As a major risk factor for heart disease, obesity has significantly hindered progress in reducing heart disease rates. Despite advancements in understanding the complexities of obesity and newer treatment options, major gaps remain between obesity research and real-world implementation in clinical practice.”
Studies show intensive lifestyle therapy is considerably more effective for weight loss than brief advice from a health care professional. However, general educational information is offered more frequently by health professionals rather than referrals to classes, programs or tangible resources for lifestyle changes. One study revealed that only 16% of health care professionals had working knowledge about evidence-based lifestyle treatments for obesity, including diet and nutrition, physical activity and intensive behavioral therapy referral. Other barriers to addressing weight loss are exacerbated by socioeconomic and racial or ethnic inequities. People of diverse races and ethnicities and people who are covered by Medicare or Medicaid are less likely to be referred to weight management programs or to have them covered by insurance.
For about 30 years, the prevalence of obesity in the US and around the world has been escalating. Recent estimates indicate more than 40% of US adults ages 20 and older are living with obesity, according to the US Centers for Disease Control and Prevention.
Research has led experts to unlock the multifactorial causes of obesity, including sociological and physiological determinants of health. Treatments for obesity have also evolved with more strategies for lifestyle modifications, medication therapy and bariatric surgery – but each treatment approach comes with challenges.
“While significant strides have been made in advancing the science to help us understand obesity, there remains a considerable gap between what we know and what happens in the doctor’s office,” said Laddu. “Health care professionals and health care systems need to find better ways to put what we know about obesity into action so more people can get the right support and treatment. Adopting new technologies and telemedicine, making referrals to community-based weight management programs to encourage behavioural change, providing social support and increasing reach and access to treatments are just some of the promising methods we could implement to unlock successful, evidence-based obesity care.”
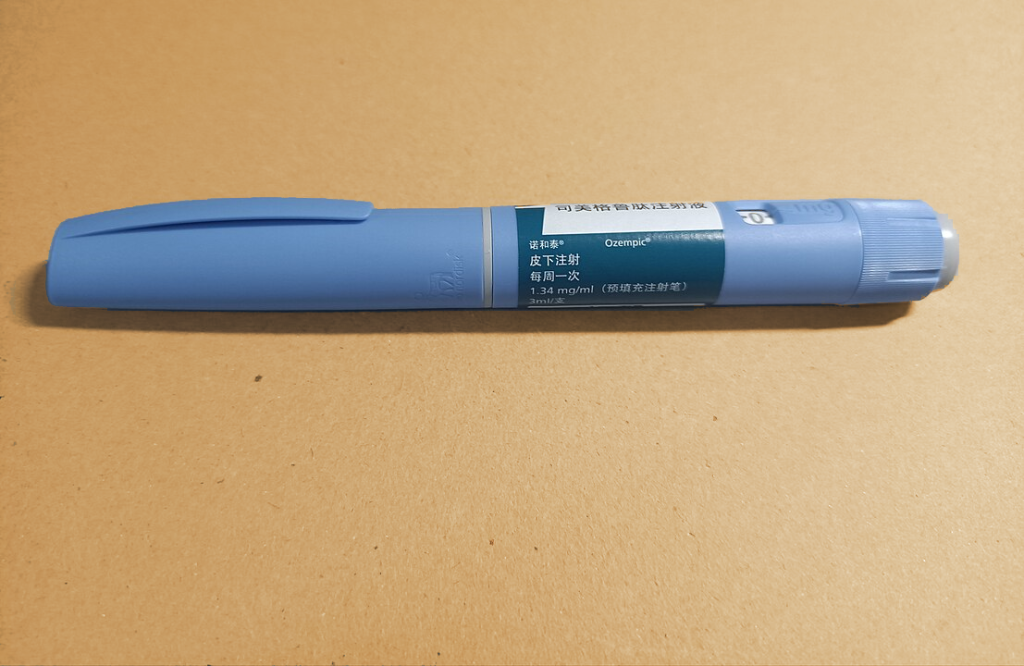
Weight loss medications
Glucagon-like peptide-1 (GLP-1) agonists, such as high-dose semaglutide and tirzepatide, are the most recently FDA-approved medications for long-term weight management, and both are associated with an average weight loss of more than 10% at six months in clinical studies. However, despite half of adults in the U.S. meeting the BMI criteria for obesity and being eligible for these medications, a small proportion of this population is currently taking them.
Weight loss surgery
In the decades since bariatric (weight loss) surgery was first introduced as an option for people with severe obesity, there have been advances in the expertise and safety of the procedures, as well as an increased understanding of the health benefits that often result after bariatric surgery. A comprehensive review of studies focused on weight loss surgeries showed that patients who underwent bariatric surgery had lower risks of cardiovascular disease and decreased risks for multiple other obesity-associated conditions, including Type 2 diabetes and high blood pressure. One challenge facing health care professionals is ensuring that the populations with the greatest needs have access to bariatric surgery in terms of costs, resources and social support.
The statement describes strategies that both address these challenges and improve how obesity-based research is incorporated into clinical care. The statement also identifies the need to develop solutions across populations in order to manage obesity at the community level. Potential improved public health policies and future research to expand patient care models and optimize the delivery and sustainability of equitable obesity-related care are suggested.
Specific approaches are highlighted in the statement to help bridge the gap between the science about obesity and clinical care, such as:
- To reach and successfully impact populations in need, health care professionals may consider how social determinants of health, including insurance type, household income, race and ethnicity, environment, health literacy, access to health-promoting resources and social supports all influence the likelihood of successful patient treatment.
- Education for health care professionals explaining the complex origins and clinical consequences of obesity is discussed. Such training should emphasize information about diagnosis, prevention and treatment of obesity. Despite the high prevalence of obesity around the world, there is a lack of education programs centered on obesity for medical professionals.
- Further evaluation of health policy changes that health care systems and insurance plans can implement and scale in order to make obesity treatment affordable for patients, especially those at high risk for adverse outcomes such as cardiovascular disease.
- A framework for delivering obesity care into clinical practice settings is reviewed, as well as efforts by some professional societies for developing interventions that make obesity treatment more accessible.
“The statement emphasises the importance of a comprehensive approach across different levels of health care delivery and public policy, along with the adoption of feasible, evidence-based strategies in clinical settings,” said Laddu. “It also underscores the need for future research and policy changes to improve current patient care models and ensure equitable access to obesity-related care for people in underrepresented groups.”
The scientific statement also provides possible solutions for how to help people in their day-to-day lives, including interventions with digital technology and access through telemedicine. However, more research is needed in obesity science and treatment. Limited understanding of the cost-effectiveness of obesity prevention and the long-term health outcomes for established therapies has hindered the implementation of obesity science into clinical settings. Cross-collaborative obesity science research between stakeholders and health economists may serve as the bridge to developing and scaling cost-effective prevention programs.
Source: American Heart Association