Scientists Discover that Mast Cells Gobble up Other Immune Cells

When it comes to allergies, mast cells are key immune system players, releasing pro-inflammatory substances in response to allergens. Now, scientists in Germany have discovered something weird: other immune cells nested inside them like Russian dolls. But how exactly did these cells wind up there?
As reported in the journal Cell, the researchers observed mast cells observed capturing and making use of neutrophils. This surprising discovery sheds new light on how our immune system works, particularly during allergic reactions.
Mast cells, residing in tissues and critical for initiating inflammation, are filled with granules containing pro-inflammatory substances. These granules are released upon encountering potential dangers, including allergens, causing allergic reactions – which for some includes innocuous materials like pollens. But despite how common allergies are, the interaction between mast cells and other immune cells at sites of allergic responses has been largely unexplored.
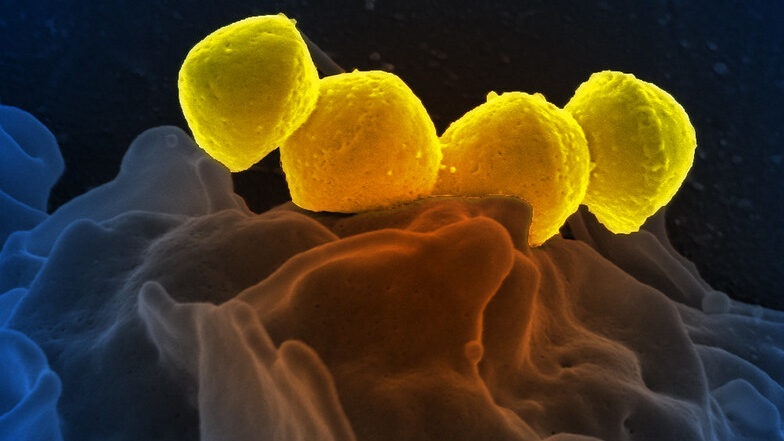
The research group at the Max Planck Institute of Immunobiology and Epigenetics in Freiburg and the University of Münster used specialised microscopy to visualise the real-time dynamics of activated mast cells and other cell types during allergic reactions in living mouse tissues. The team discovered a surprising interaction: neutrophils were found inside mast cells.
“We could hardly believe our eyes: living neutrophils were sitting inside living mast cells. This phenomenon was completely unexpected and probably would not have been discovered in experiments outside a living organism and highlights the power of intravital microscopy,” says Tim Lämmermann, research leader and Director at the Institute of Medical Biochemistry at the University of Münster.
Pulling a neutrophil trick to trap neutrophils
Neutrophils are frontline immune system defenders, responding quickly and broadly to potential threats. They circulate in the blood and quickly exit blood vessels at sites of inflammation. They are well-equipped to combat pathogens by engulfing the invaders, releasing antimicrobial substances, or forming web-like traps known as ‘neutrophil extracellular traps’. Additionally, neutrophils can communicate with each other and form cell swarms to combine their individual functions for the protection of healthy tissue. While much is known about neutrophils’ role in infections and sterile injuries, their role in inflammation caused by allergic reactions is less understood.
“It quickly became clear that the double-pack immune cells were no mere coincidence. We wanted to understand how mast cells trap their colleagues and why they do it,” explains Michael Mihlan, first and co-corresponding author of the study. Once the team was able to mimic the neutrophil trapping observed in living tissue in cell culture, they we were able to identify the molecular pathways involved in this process. The researchers found that mast cells release leukotriene B4, a substance commonly used by neutrophils to initiate their own swarming behaviour.
By secreting this substance, mast cells attract neutrophils. Once the neutrophils are close enough, mast cells engulf them into a vacuole, forming a cell-in-cell structure that the researchers refer to as ‘mast cell intracellular trap’ (MIT). “It is ironic that neutrophils, which create web-like traps made of DNA and histones to capture microbes during infections, are now trapped themselves by mast cells under allergic conditions,” says Tim Lämmermann.
Recycled neutrophils to boost mast cell function
With the help of an international team, the researchers confirmed the formation of MITs in human samples and investigated the fate of the two cell types involved after trapping. They found that trapped neutrophils eventually die, and their remains get stored inside mast cells. “This is where the story takes an unexpected turn. Mast cells can recycle the material from the neutrophils to boost their own function and metabolism. In addition, mast cells can release the newly acquired neutrophil components in a delayed manner, triggering additional immune responses and helping to sustain inflammation and immune defense”, says Michael Mihlan.
“This new understanding of how mast cells and neutrophils work together adds a whole new layer to our knowledge of allergic reactions and inflammation. It shows that mast cells can use neutrophils to boost their own capabilities – an aspect that could have implications for chronic allergic conditions where inflammation occurs repeatedly,” says Tim Lämmermann. The researchers have already begun investigating this interaction in mast cell-mediated inflammatory diseases in humans, exploring whether this discovery could lead to new approaches to treating allergies and inflammatory diseases.
Source: Max Planck Institute of Immunobiology and Epigenetics