Ancient Medicinal Minerals Inspire New Tissue Repair Technology
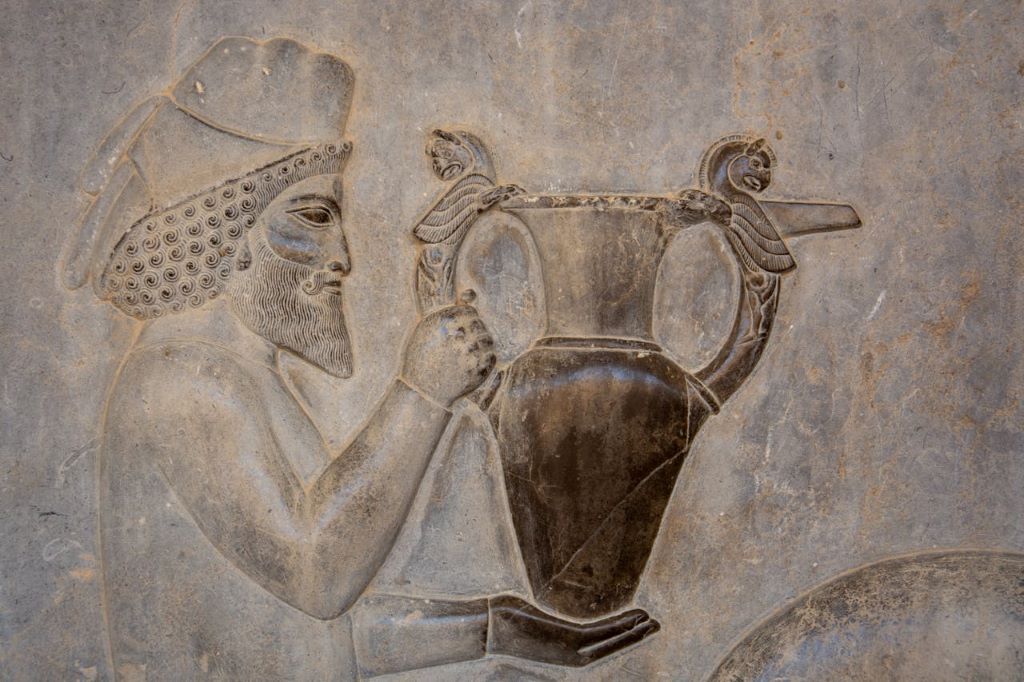
For centuries, civilizations have used naturally occurring, inorganic materials for their perceived healing properties. Egyptians thought green copper ore helped eye inflammation, the Chinese used cinnabar for heartburn, and Native Americans used clay to reduce soreness and inflammation.
Today, researchers at Texas A&M University are still discovering ways that inorganic materials can be used for healing.
In two recently published articles, Dr Akhilesh Gaharwar, a Tim and Amy Leach Endowed Professor in the Department of Biomedical Engineering, and Dr Irtisha Singh, assistant professor in the Department of Cell Biology and Genetics, uncovered new ways that inorganic materials can aid tissue repair and regeneration.
The first article, published in Acta Biomaterialia, explains that cellular pathways for bone and cartilage formation can be activated in stem cells using inorganic ions. The second article, published in Advanced Science, explores the usage of mineral-based nanomaterials, specifically 2D nanosilicates, to aid musculoskeletal regeneration.
“These investigations apply cutting-edge, high-throughput molecular methods to clarify how inorganic biomaterials affect stem cell behavior and tissue regenerative processes,” Singh said.
The ability to induce natural bone formation holds promise for improvements in treatment outcomes, patient recovery times and the reduced need for invasive procedures and long-term medication.
“Enhancing bone density and formation in patients with osteoporosis, for example, can help mitigate the risks of fractures, lead to stronger bones, improve quality of life and reduce healthcare costs,” Gaharwar said. “These insights open up exciting prospects for developing next-generation biomaterials that could provide a more natural and sustainable approach to healing.”
Gaharwar said the newfound approach differs from current regeneration methods that rely on organic or biologically derived molecules and provides tailored solutions for complex medical issues.
“One of the most significant findings from our research is the ability of these nanosilicates to stabilise stem cells in a state conducive to skeletal tissue regeneration,” he said. “This is crucial for promoting bone growth in a controlled and sustained manner, which is a major challenge in current regenerative therapies.”
Gaharwar recently received a grant for his work in using inorganic biomaterials in conjunction with 3D bioprinting techniques to design custom bone implants for reconstructive injuries.
“In reconstructive surgery, particularly for craniofacial defects, induced bone growth is crucial for restoring both function and appearance, vital for essential functions like chewing, breathing and speaking,” he said. “Inducing bone formation has several critical applications in orthopaedics and dentistry.”
“This approach not only bridges ancient practices with modern scientific methods but also minimises the use of protein therapeutics, which carry risks of inducing abnormal tissue growth and cancerous formations,” Gaharwar said. “Collectively, these findings elucidate the potential of inorganic biomaterials to act as powerful mediators in tissue engineering and regenerative strategies, marking a significant step forward in the field.”
Source: Texas A&M University





