New Findings on Cardiovascular Risk, Menopause and Migraines Ease Concerns

Research suggesting a link between migraines and menopause symptoms and cardiovascular disease has gotten a lot of attention. But a pair of new studies in the journal Menopause suggest that most women experiencing these symptoms can rest easier, especially if they don’t have both migraines and long-term hot flashes and night sweats.
Instead, they should focus on tackling the other factors that can raise their cardiovascular risk by getting more sleep, exercise and healthy foods, quitting tobacco, and minding their blood pressure, blood sugar, cholesterol and weight.
For women who have experienced both migraines and hot flashes or night sweats over many years, one of the new studies does suggest an extra level of cardiovascular risk.
That makes heart disease and stroke prevention even more important in this group, says study leader Catherine Kim, MD, MPH, of the University of Michigan.
And for women currently in their 20s and 30s who experience migraines, the new research suggests that they might be heading for a higher risk of long-term menopause-related symptoms when they get older.
Long-term study yields important insights
Kim and her colleagues at Michigan Medicine, U-M’s academic medical centre, published the new pair of studies based on an in-depth analysis of data from a long-term study of more than 1900 women who volunteered to have regular physical exams and blood tests, and to take yearly health surveys, when they were in their late teens to early 30s.
Those women, now in their 50s and 60s, have provided researchers with a priceless view of what factors shape health in the years leading up to menopause and beyond, through their continued participation in the CARDIA study.
“The anxiety and dread that women with migraines and menopausal symptoms feel about cardiovascular risk is real – but these findings suggest that focusing on prevention, and correcting unhealthy habits and risk factors, could help most women,” said Kim, who is an associate professor of internal medicine at U-M and a primary care physician.
“For the subgroup with both migraines and early persistent hot flashes and night sweats, and for those currently experiencing migraines in their early adulthood, these findings point to an added need to control risks, and address symptoms early,” she adds.
Just over 30% of the middle-aged women in the study reported they had persistent hot flashes and night sweats, which together are called vasomotor symptoms or VMS because they relate to changes in the diameter of blood vessels.
Of them, 23% had reported also having migraines. This was the only group for whom Kim and her colleagues found extra risk of stroke, heart attack or other cardiovascular events that couldn’t be explained by other risk factors that have long been known to be linked to cardiovascular problems.
In addition to those with persistent vasomotor symptoms starting in their 40s or before, 43% of the women in the study had minimal levels of such symptoms in their 50s, and 27% experienced an increase in VMS over time into their 50s and early 60s.
The latter two groups had no excess cardiovascular risk once their other risk factors were taken into account, whether or not they had migraines.
Use of hormone-based birth control and estrogen to address medical issues did not affect this risk.
Controlling destiny
In the study of data from the same women in their earlier stages of life, the researchers found that the biggest factors in predicting which ones would go on to have persistent hot flashes and night sweats were having migraines, having depression, and smoking cigarettes, as well as being Black or having less than a high school education.
“These two studies, taken together, underscore that not all women have the same experiences as they grow older, and that many can control the risk factors that might raise their chances of heart disease and stroke later in life,” said Kim.
“In other words, women can do a lot to control their destiny when it comes to both menopause symptoms and cardiovascular diseases.”
She notes that the American Heart Association calls these risk factors the “Essential 8” and offers guides for what women, men and even children and teens can do to address them.
Evolving knowledge and treatment
The long-term study that the two new findings come from was specifically designed to look at cardiovascular risks when it launched in the mid-1980s. CARDIA stands for Coronary Artery Risk Development in Young Adults.
Back in the 80s, knowledge about the biology of blood vessels, down to the cellular and molecular level, was nowhere near where it is today. Both vasomotor symptoms in menopause and migraines have to do with blood vessel contraction and dilation.
But decades of research has shown the microscopic impacts on blood vessels of years of smoking, poor sleep, poor eating habits and lack of activity, as well as a person’s genetic inheritance, life experiences and hormonal history.
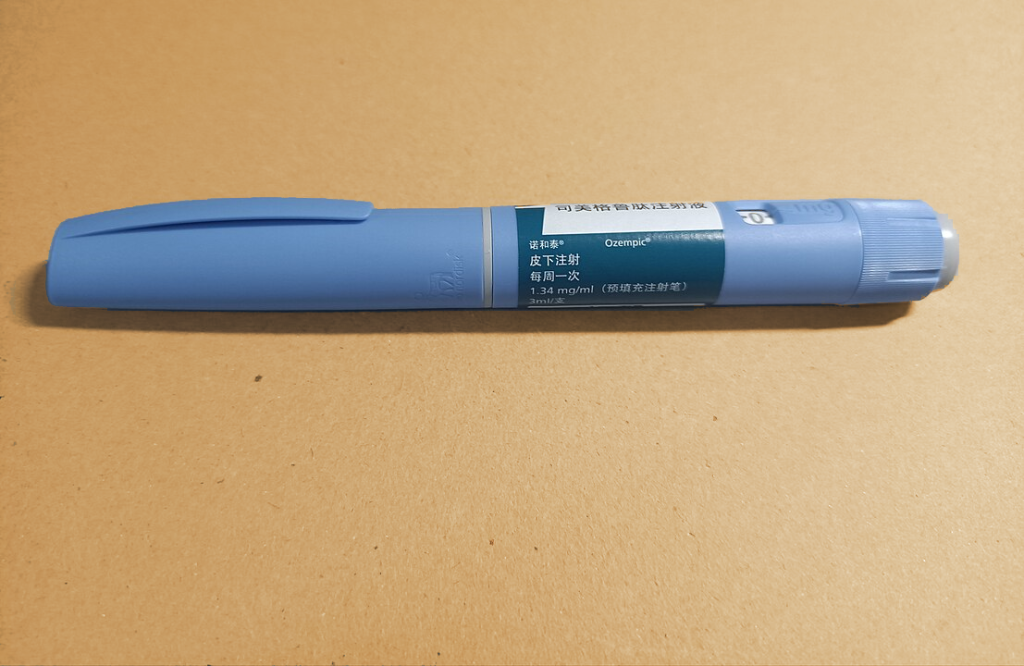
Newer injectable migraine medications called calcitonin gene-related peptide (CGRP) antagonists have reached the market in recent years. Using monoclonal antibodies, they target a key receptor on the surface of blood vessel cells to prevent migraines and cluster headaches. But they are expensive and not covered by insurance for all people with migraines.
While the new study is based on data from years before these medications became available, Kim said she recommends them to her patients with persistent migraines, as well as working with them to understand what triggers their migraines and how to use other medications including pain relievers and antiseizure medications to prevent them.
She also notes that the paper on future risk of persistent hot flashes and night sweats echoes the recent trend of using antidepressant medications to try to ease these menopause effects.
Kim also says that evidence has grown about the importance of healthy sleep habits for reducing hot flashes, as well the short-term use of oestradiol-based hormone therapy patches, which have not been shown to have a link to cardiovascular risk. And, she notes that research has not shown any over-the-counter supplement or herbal remedy to be effective, and that these are far less regulated than medications.