How does Oxygen Depletion Disrupt Memory Formation in the Brain?
Scientists identify a positive molecular feedback loop which could explain stroke-induced memory loss.
In learning, neurons communicate with each other, and the connections between them getting stronger with repetition. This is known as long-term potentiation or LTP.
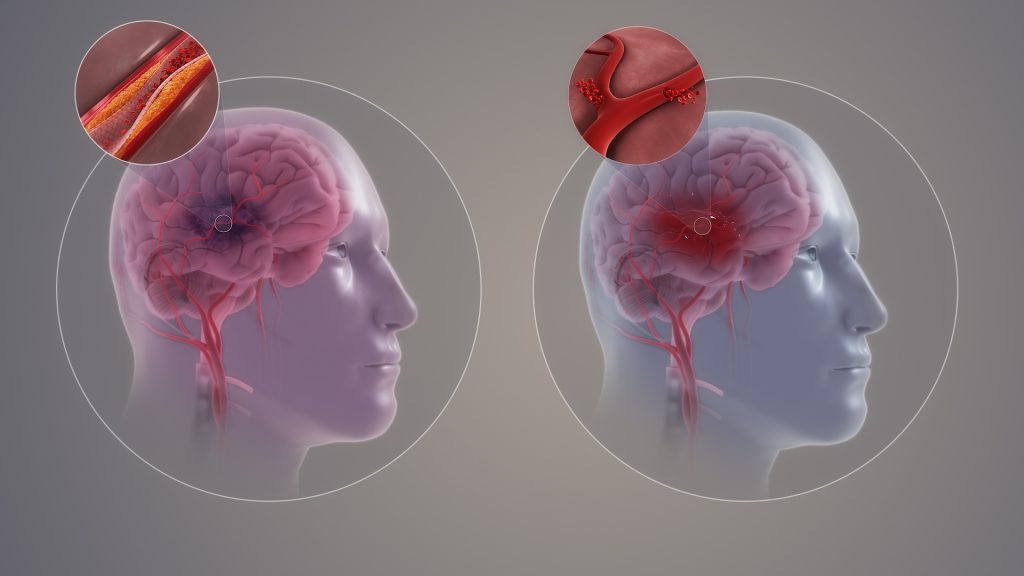
Another type of LTP occurs when the brain is deprived of oxygen temporarily – anoxia-induced long-term potentiation or aLTP. aLTP blocks the former process, thereby impairing learning and memory. Therefore, some scientists think that aLTP might be involved in memory problems seen in conditions like stroke.
Researchers at the Okinawa Institute of Science and Technology (OIST) and their collaborators have studied the aLTP process in detail. They found that maintaining aLTP requires the amino acid glutamate, which triggers nitric oxide (NO) production in both neurons and brain blood vessels. This process forms a positive glutamate-NO-glutamate feedback loop. Their study, published in iScience, indicates that the continuous presence of aLTP could potentially hinder the brain’s memory strengthening processes and explain the memory loss observed in certain patients after experiencing a stroke.
The brain’s response to low oxygen
When there is a lack of oxygen in the brain, the neurotransmitter glutamate is released from neurons in large amounts. This increased glutamate causes the production of NO. NO produced in neurons and brain blood vessels boosts glutamate release from neurons during aLTP. This glutamate-NO-glutamate loop continues even after the brain gets enough oxygen.
“We wanted to know how oxygen depletion affects the brain and how these changes occur,” stated Dr Han-Ying Wang, a researcher in the former Cellular and Molecular Synaptic Function Unit at OIST and lead author of the study,. “It’s been known that nitric oxide is involved in releasing glutamate in the brain when there is a shortage of oxygen, but the mechanism was unclear.”
During a stroke, when the brain is deprived of oxygen, amnesia – the loss of recent memories – can be one of the symptoms. Investigating the effects of oxygen deficiency on the brain is important because of the potential medicinal benefits. “If we can work out what’s going wrong in those neurons when they have no oxygen, it may point in the direction of how to treat stroke patients,” Dr Patrick Stoney, a scientist in OIST’s Sensory and Behavioral Neuroscience Unit, explained.
Brain tissues from mice were placed in a saline solution, mimicking the natural environment in the living brain. Normally, this solution is oxygenated to meet the high oxygen demands of brain tissue. However, replacing the oxygen with nitrogen allowed the researchers to deprive the cells of oxygen for precise lengths of time.
The tissues were then examined under a microscope and electrodes were placed on them to record electrical activity of the individual cells. The cells were stimulated in a way that mimics how they would be stimulated in living mice.
Stopping memory and learning activity

The scientists found that maintaining aLTP requires NO production in both neurons and in blood vessels in the brain. Collaborating scientists from OIST’s Optical Neuroimaging Unit showed that in addition to neurons and blood vessels, aLTP requires the activity of astrocytes, another type of brain cell. Astrocytes connect and support communication between neurons and blood vessels.
“Long-term maintenance of aLTP requires continuous synthesis of nitric oxide. NO synthesis is self-sustaining, supported by the NO-glutamate loop, but blocking molecular steps for NO-synthesis or those that trigger glutamate release eventually disrupt the loop and stop aLTP,” Prof. Tomoyuki Takahashi, leader of the former Cellular and Molecular Synaptic Function Unit at OIST, explained.
Notably, the cellular processes that support aLTP are shared by those involved in memory strengthening and learning (LTP). When aLTP is present, it hijacks molecular activities required for LTP and removing aLTP can rescue these memory enhancing mechanisms. This suggests that long-lasting aLTP may obstruct memory formation, possibly explaining why some patients have memory loss after a short stroke.
Prof Takahashi emphasised that the formation of a positive feedback loop formed between glutamate and NO when the brain is temporarily deprived of oxygen is an important finding. It explains long-lasting aLTP and may offer a solution for memory loss caused by a lack of oxygen.




