Healthcare Trends to Watch in 2025

Quicknews takes a look at some of the big events and concerns that defined healthcare 2024, and looks into its crystal ball identify to new trends and emerging opportunities from various news and opinion pieces. There’s a lot going on right now: the battle to make universal healthcare a reality for South Africans, growing noncommunicable diseases and new technologies and treatments – plus some hope in the fight against HIV and certain other diseases.
1. The uncertainty over NHI will continue
For South Africa, the biggest event in healthcare was the signing into law of the National Health Insurance (NHI) by President Ramaphosa in May 2024, right before the elections. This occurred in the face of stiff opposition from many healthcare associations. It has since been bogged down in legal battles, with a section governing the Certificate of Need to practice recently struck down by the High Court as it infringed on at least six constitutional rights.
Much uncertainty around the NHI has been expressed by various organisation such as the Health Funders Association (HFA). Potential pitfalls and also benefits and opportunities have been highlighted. But the biggest obstacle of all is the sheer cost of the project, estimated at some R1.3 trillion. This would need massive tax increases to fund it – an unworkable solution which would see an extra R37 000 in payroll tax. Modest economic growth of around 1.5% is expected for South Africa in 2025, but is nowhere near creating enough surplus wealth to match the national healthcare of a country like Japan. And yet, amidst all the uncertainty, the healthcare sector is expected to do well in 2025.
Whether the Government of National Unity (GNU) will be able to hammer out a workable path forward for NHI remains an open question, with various parties at loggerheads over its implementation. Public–private partnerships are preferred by the DA and groups such as Solidarity, but whether the fragile GNU will last long enough for a compromise remains anybody’s guess.
It is reported that latest NHI proposal from the ANC includes forcing medical aid schemes to lower their prices by competing with government – although Health Minister Aaron Motsoaledi has dismissed these reports. In any case, medical aid schemes are already increasing their rates as healthcare costs continue to rise in what is an inexorable global trend – fuelled in large part by ageing populations and increases in noncommunicable diseases.
2. New obesity treatments will be developed
Non-communicable diseases account for 56% of deaths in South Africa, and obesity is a major risk factor, along with hypertension and hyperglycaemia, which are often comorbid. GLP-1 agonists were all over the news in 2023 and 2024 as they became approved in certain countries for the treatment of obesity. But in South Africa, they are only approved for use in obesity with a diabetes diagnosis, after diet and exercise have failed to make a difference, with one exception. Doctors also caution against using them as a ‘silver bullet’. Some are calling for cost reductions as they can be quite expensive; a generic for liraglutide in SA is expected in the next few years.
Further on the horizon, there are a host of experimental drugs undergoing testing for obesity treatment, according to a review published in Nature. While GLP-1 remains a target for many new drugs, others focus on gut hormones involved in appetite: GIP-1, glucagon, PYY and amylin. There are 5 new drugs in Phase 3 trials, expected variously to finish between 2025 and 2027, 10 drugs in Phase 2 clinical trials and 18 in Phase 1. Some are also finding applications beside obesity. The GLP-1 agonist survodutide, for example have received FDA approval not for obesity but for liver fibrosis.
With steadily increasing rates of overweight/obesity and disorders associated with them, this will continue to be a prominent research area. In the US, where the health costs of poor diet match what consumers spend on groceries, ‘food as medicine’ has become a major buzzword as companies strive to deliver healthy nutritional solutions. Retailers are providing much of the push, and South Africa is no exception. Medical aid scheme benefits are giving way to initiatives such as Pick n Pay’s Live Well Club, which simply offers triple Smart Shopper points to members who sign up.
Another promising approach to the obesity fight is precision medicine, which factors in many data about the patient to identify the best interventions. This could include detailed study of energy balance regulation, helping to select the right antiobesity medication based on actionable behavioural and phsyiologic traits. Genotyping, multi-omics, and big data analysis are growing fields that might also uncover additional signatures or phenotypes better responsive to certain interventions.
3. AI tools become the norm
Wearable health monitoring technology has gone from the lab to commonly available consumer products. Continued innovation in this field will lead to cheaper, more accurate devices with greater functionality. Smart rings, microneedle patches and even health monitoring using Bluetooth earphones such as Apple’s Airpods show how these devices are becoming smaller and more discrete. But health insurance schemes remain unconvinced as to their benefits.
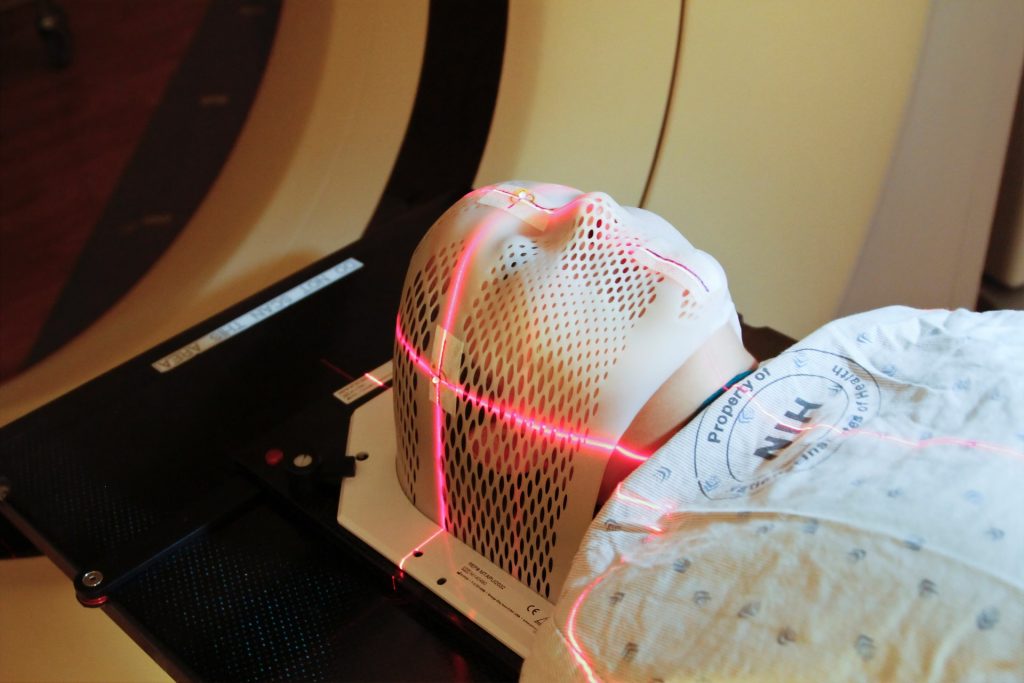
After making a huge splash in 2024 as it rapidly evolved, AI technology is now maturing and entering a consolidation phase. Already, its use has become commonplace in many areas: the image at the top of the article is AI-generated, although it took a few attempts with the doctors exhibiting polydactyly and AI choosing to write “20215” instead of “2025”. An emerging area is to use AI in patient phenotyping (classifying patients based on biological, behavioural, or genetic attributes) and digital twins (virtual simulations of individual patients), enabling precision medicine. Digital twins for example, can serve as a “placebo” in a trial of a new treatment, as is being investigated in ALS research.
Rather than replacing human doctors, it is likely that AI’s key application is reducing lowering workforce costs, a major component of healthcare costs. Chatbots, for example, could engage with patients and help them navigate the healthcare system. Other AI application include tools to speed up and improve diagnosis, eg in radiology, and aiding communication within the healthcare system by helping come up with and structure notes.
4. Emerging solutions to labour shortages
Given the long lead times to recruit and train healthcare workers, 2025 will not likely see any change to the massive shortages of all positions from nurses to specialists.
At the same time, public healthcare has seen freezes on hiring resulting in the paradoxical situation of unemployed junior doctors in a country desperately in need of more doctors – 800 at the start of 2024 were without posts. The DA has tabled a Bill to amend the Health Professions Act at would allow private healthcare to recruit interns and those doing community service. Critics have pointed out that it would exacerbate the existing public–private healthcare gap.
But there are some welcome developments: thanks to a five-year plan from the Department of Health, family physicians in SA are finally going to get their chance to shine and address many problems in healthcare delivery. These ‘super generalists’ are equipped with a four-year specialisation and are set to take up roles as clinical managers, leading multi-disciplinary district hospital teams.
Less obvious is where the country will be able to secure enough nurses to meet its needs. The main challenge is that nurses, especially specialist nurses, are ageing – and it’s not clear where their replacements are coming from. In the next 15 years, some 48% of the country’s nurses are set to retire. Coupled with that is the general consensus that the new nursing training curriculum is a flop: the old one, from 1987 to 2020, produced nurses with well-rounded skills, says Simon Hlungwani, president of the Democratic Nursing Organisation of South Africa (Denosa). There’s also a skills bottleneck: institutions like Baragwanath used to cater for 300 students at a time, now they are only approved to handle 80. The drive for recruitment will also have to be accompanied by some serious educational reform to get back on track.
5. Progress against many diseases
Sub-Saharan Africa continues to drive declines in new HIV infections. Lifetime odds of getting HIV have fallen by 60% since the 1995 peak. It also saw the largest decrease in population without a suppressed level of HIV (PUV), from 19.7 million people in 2003 to 11.3 million people in 2021. While there is a slowing in the increase of population living with HIV, it is predicted to peak by 2039 at 44.4 million people globally. But the UNAIDS HIV targets for 2030 are unlikely to be met.
As human papillomavirus (HPV) vaccination programmes continue, cervical cancer deaths in young women are plummeting, a trend which is certain to continue.
A ‘new’ respiratory virus currently circulating in China will fortunately not be the next COVID. Unlike SARS-CoV-2, human metapneumovirus (HMPV) has been around for decades, and only causes a few days of mild illness, with bed rest and fluids as the primary treatment. The virus has limited pandemic potential, according to experts.