High Uric Acid Levels Linked to Mortality in Children with Severe Malaria

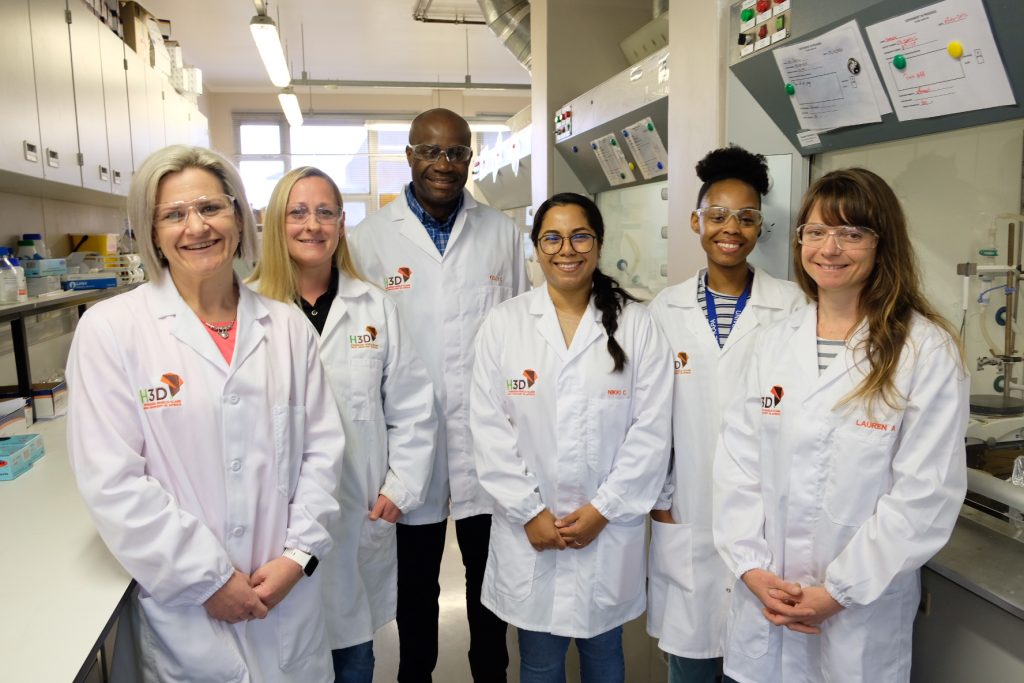
Indiana University School of Medicine researchers and their collaborators in Uganda at the Makerere University School of Medicine have uncovered a significant connection between elevated uric acid levels and life-threatening outcomes in children with severe malaria.
Published in Nature Medicine, the study identified hyperuricaemia – high uric acid levels – as a potential contributor to increased mortality and long-term neurodevelopmental challenges in children with severe malaria. These findings open the door to future research that could improve treatment strategies for children affected by severe malaria, a disease caused by mosquito-transmitted parasites and a leading cause of death in African children.
“Our findings show that hyperuricemia is strongly associated with death in the hospital and after discharge and with long-term cognitive impairment in children with severe malaria,” said Chandy C. John, MD, paediatrics professor at IU School of Medicine, who co-led the study. “We also showed several mechanisms by which hyperuricaemia may lead to these outcomes, suggesting that hyperuricaemia is not just associated with bad outcomes but may contribute to them.”
The researchers analysed data from two independent groups of children with severe malaria in Uganda and found that 25% had hyperuricaemia. This condition is caused by excess uric acid, which is a harmful body waste substance found in blood. The primary drivers of hyperuricaemia in study participants were broken-down infected red blood cells and kidney injury, which reduces the body’s ability to get rid of the extra uric acid.
In the study, hyperuricemia was linked to four negative outcomes in children with severe malaria: serious health complications like coma and anaemia, a higher risk of death during hospitalisation, a higher risk of death after discharge from the hospital, and long-term cognitive impairment in survivors.
The study also revealed that children with hyperuricemia had more harmful gut bacteria, which can cross the injured gut lining and cause sepsis. Together, these findings highlight a need for clinical trials to test the effectiveness of uric acid-lowering medications as an additional treatment for severe malaria.
“Additional studies are needed to determine whether lowering uric acid in children with severe malaria might reduce hospital deaths, post-discharge deaths and long-term cognitive impairment,” said Andrea Conroy, PhD, associate professor of paediatrics at the IU School of Medicine and co-leader of the study. “Our hope is that these studies will provide new insights and potentially lead to improved treatments that save lives.”
This research builds on the team’s recent discovery of partial resistance to the primary treatment for malaria in African children with severe malaria. Both studies underscore the importance of prioritizing new strategies to combat malaria, which affected 263 million people and caused nearly 600,000 deaths worldwide in 2023.
Source: Indiana University