A Novel Pathway with Potential to Slow the Progression of Pulmonary Fibrosis
Researchers have found a potential new way to slow the progression of lung fibrosis and other fibrotic diseases by inhibiting the expression or function of Piezo2, a receptor that senses mechanical forces in tissues including stress, strain, and stiffness. The new study in The American Journal of Pathology, published by Elsevier, sheds light on the underlying mechanisms of pulmonary fibrotic diseases and identifies potential new targets and options for therapy to improve patients’ outcomes.
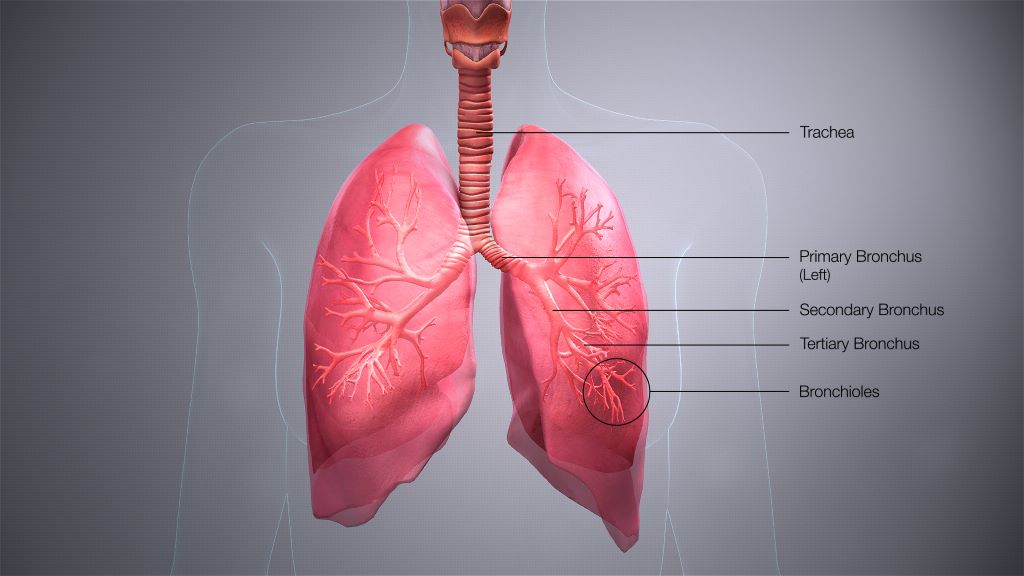
Pulmonary fibrotic diseases are a group of conditions that cause significant morbidity and sometimes mortality. Idiopathic pulmonary fibrosis (IPF) is a devastating progressive fibrotic lung disease with a median survival of 2.9 years from diagnosis. Lung fibrosis results in dramatic mechanical changes including increased stiffness in the tissue that cells can sense and respond to, making it difficult for the lungs to expand and contract properly during breathing.
Piezo channels are a newly discovered receptor that are sensitive to mechanical signals. Since the 2021 Nobel Prize in Medicine was awarded to Dr Ardem Patapoutian for the discovery of Piezo channels in 2010, interest has increased in their role in tissue homeostasis and disease outside of neuronal signalling, however, little has been published on their possible role in fibrotic lung diseases. A group of researchers driven to understand how mechanical forces in lung tissue contribute to and drive pulmonary fibrosis investigated the role of Piezo2 in pulmonary fibrosis using donor tissue from patients with IPF, mouse models of lung fibrosis, cell culture investigation of lung cells (fibroblasts) that create the fibrosis lesions, and by examining publicly available RNAseq datasets from other research groups.
Investigators found that:
- Piezo2 is highly expressed in human lung tissue from patients with IPF and in multiple (different) mouse models of lung fibrosis.
- Piezo2 is highly expressed in primary human lung fibroblasts in culture, the cells that are believed to play key roles in producing fibrosis in tissues (by proliferating and laying down matrix proteins, creating scar-like features).
- Lung fibroblasts grown on stiffer substrates are reprogrammed to be more profibrotic, by proliferating, producing extra matrix proteins, and differentiating to scar-forming myofibroblasts.
- Inhibition of Piezo2 with either RNA silencing or a peptide inhibitor, to prevent them from sensing the stiffness of their environment, reduces profibrotic programming.
Lead investigator Patricia J. Sime, MD, Division of Pulmonary Disease and Critical Care Medicine, Virginia Commonwealth University, says, “We are excited to report that this research that suggests inhibiting expression or function of Piezo2 could be a potential new therapeutic route to treating lung fibrosis and other fibrotic diseases. This is especially important as there is an unmet need for additional therapies for fibrotic diseases.”
Despite the introduction of nintedanib and pirfenidone for therapy of some fibrotic lung diseases, pulmonary fibrosis can remain challenging to effectively treat. This is in part because lung cells can be driven to a profibrotic phenotype by multiple pathways that reinforce each other, so that targeting one pathway alone may not be effective to slow or stop disease progression.
First author Margaret A.T. Freeberg, PhD, Division of Pulmonary Disease and Critical Care Medicine, Virginia Commonwealth University, continues, “Some types of lung fibrosis have been very difficult to treat. For example, IPF is a form of pulmonary fibrosis that often progresses. While there have been advances in therapy, the approved medications for IPF can slow, but do not always halt progression. One of the reasons that fibrosis can be difficult to effectively treat may be explained by the multiple profibrotic disease pathways that reinforce each other. Blocking Piezo2 signaling to prevent fibroblast reprogramming represents a new pathway we can target in our fight against fibrosis.”
Dr. Sime concludes, “This research identifies mechanical forces and a new specific target (Piezo2) that we can block to prevent fibrotic reprogramming of some lung cells. We believe this points to Piezo2 as an important new therapeutic target that might (by itself or in combination with other therapies) slow the progression of pulmonary fibrosis in our patients. Many new investigational drugs that target pulmonary fibrosis receive orphan drug designation from the FDA, and this may accelerate development and increase interest from pharmaceutical partners.”
Source: Elsevier