Deep Depletion of Blood Lipoprotein(a) Levels with New Drug
In a new study, researchers found that a new drug under development, zerlasiran, depleted levels of lipoprotein(a) by more than 80% in participants with increased cardiovascular risk. The drug was well tolerated and the findings, published in JAMA Network, suggest that this could be the first viable treatment for elevated levels of lipoprotein(a).
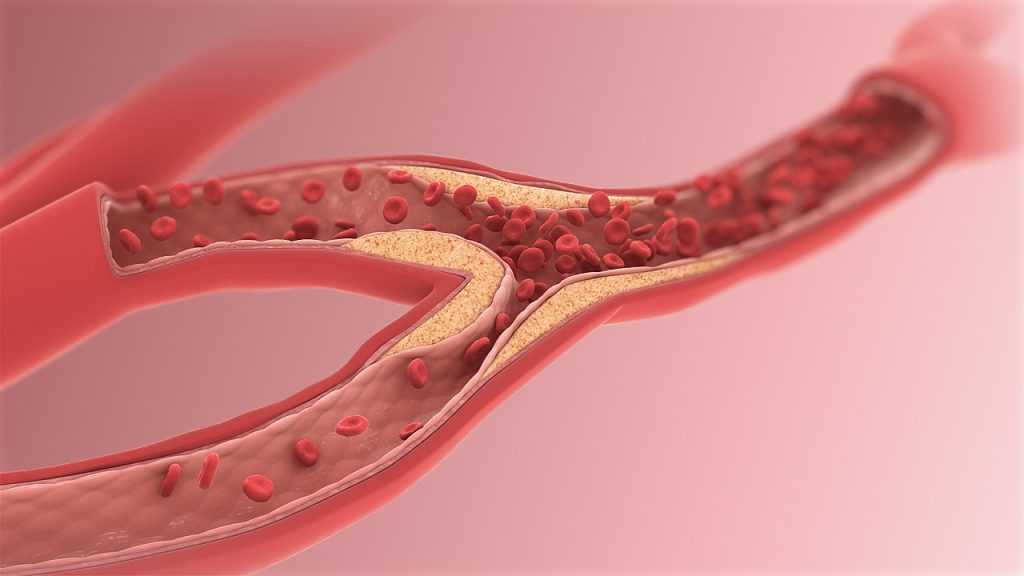
Elevated levels of lipoprotein(a) (LPa) – a type of cholesterol – is a genetic risk factor for cardiovascular disease. Present in 20% of the population, it increases the risk of atherosclerotic cardiovascular disease (ASCVD) and aortic stenosis. Currently, there are no interventions which can bring down high LPa levels: it is unresponsive to diet, exercise, and other lifestyle changes and there is no available drug.
Zerlasiran, a small-interfering RNA that targets synthesis of LPa serum concentration, was developed to fill this gap. It is effectively a gene silencer that shuts down LPA, a gene which produces a protein found only in LPa. This in turn is expected to reduce cardiovascular risk.
A phase I clinical trial had shown that zerlasiran was safe and effective.
For the study, researchers enrolled 178 patients (average age 63.7 years, 46 female) with ASCVD and LPa concentrations greater than or equal to 125nmol/L. They were randomised to subcutaneously receive zerlasiran 300mg or 450mg, or a placebo, every 16 or every 24 weeks. The least-squares mean placebo-adjusted time-averaged percent change in LPa serum concentrations was −85.6%, −82.8%, and −81.3% for the 450mg every 24 weeks, 300mg every 16 weeks, and 300 mg every 24 weeks groups, respectively. The most common adverse events were injection site reactions, with mild pain occurring in 2.3% to 7.1% of participants in the first day following drug administration. There were 20 serious adverse events in 17 patients, none considered related to the study drug. For the group receiving a 300mcg dose every 16 weeks, it was found that even at the 60 week follow-up, 28 weeks after the last administration, that lipoprotein(a) serum concentrations were still 60% lower than baseline.



