Research Identifies Beneficial Genetic Changes in Regular Blood Donors

Researchers at the Francis Crick Institute have identified genetic changes in blood stem cells from frequent blood donors that support the production of new, non-cancerous cells.
Understanding the differences in the mutations that accumulate in our blood stem cells as we age is important to understand how and why blood cancers develop and hopefully how to intervene before the onset of clinical symptoms.
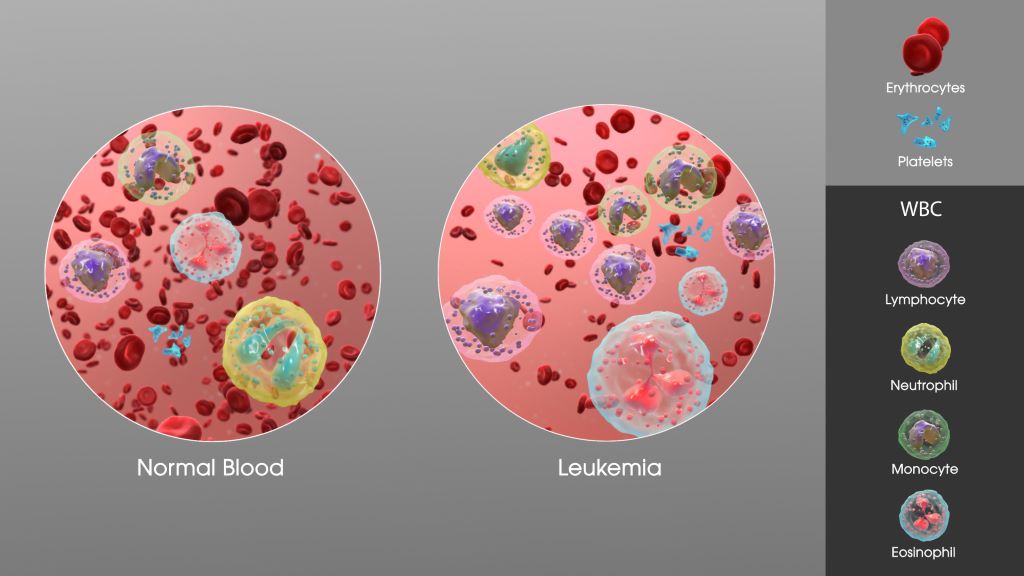
As we age, stem cells in the bone marrow naturally accumulate mutations and with this, we see the emergence of clones, which are groups of blood cells that have a slightly different genetic makeup. Sometimes, specific clones can lead to blood cancers like leukaemia.
When people donate blood, stem cells in the bone marrow make new blood cells to replace the lost blood and this stress drives the selection of certain clones.
Blood donation impacts makeup of cell populations
In research published in Blood, the team at the Crick, in collaboration with scientists from the DKFZ in Heidelberg and the German Red Cross Blood Donation Centre, analysed blood samples taken from over 200 frequent donors – (three donations a year over 40 years, more than 120 times in total) – and sporadic control donors who had donated blood less than five times in total.
Samples from both groups showed a similar level of clonal diversity, but the makeup of the blood cell populations was different.
For example, both sample groups contained clones with changes to a gene called DNMT3A, which is known to be mutated in people who develop leukaemia. Interestingly, the changes to this gene observed in frequent donors were not in the areas known to be preleukaemic.
A balancing act
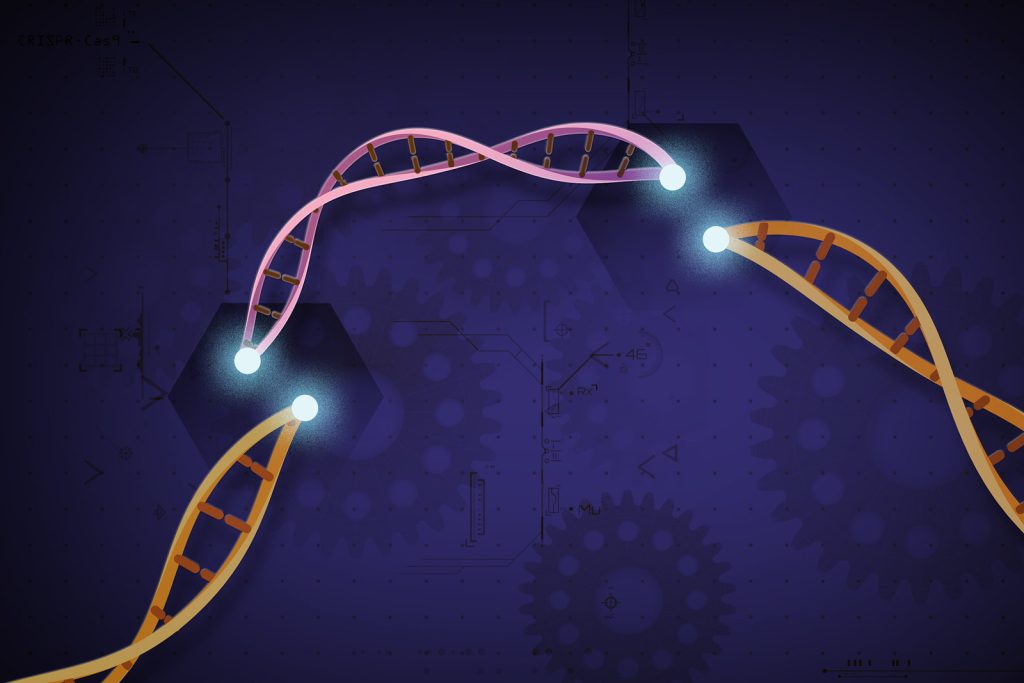
To understand this better, the Crick researchers edited DNMT3A in human stem cells in the lab. They induced the genetic changes associated with leukaemia and also the non-preleukaemic changes observed in the frequent donor group.
They grew these cells in two environments: one containing erythropoietin (EPO), a hormone that stimulates red blood cell production which is increased after each blood donation, and another containing inflammatory chemicals to replicate an infection.
The cells with the mutations commonly seen in frequent donors responded and grew in the environment containing EPO and failed to grow in the inflammatory environment. The opposite was seen in the cells with mutations known to be preleukaemic.
This suggests that the DNMT3A mutations observed in the frequent donors are mainly responding to the physiological blood loss associated with blood donation.
Finally, the team transplanted the human stem cells carrying the two types of mutations into mice. Some of these mice had blood removed and then were given EPO injections to mimic the stress associated with blood donation.
The cells with the frequent donor mutations grew normally in control conditions and promoted red blood cell production under stress, without cells becoming cancerous. In sharp contrast, the preleukaemic mutations drove a pronounced increase in white blood cells in both control or stress conditions.
The researchers believe that regular blood donation is one type of activity that selects for mutations that allow cells to respond well to blood loss, but does not select the preleukaemic mutations associated with blood cancer.
Interactions of genes and the environment
Dominique Bonnet, Group Leader of the Haematopoietic Stem Cell Laboratory at the Crick, and senior author, said: “Our work is a fascinating example of how our genes interact with the environment and as we age. Activities that put low levels of stress on blood cell production allow our blood stem cells to renew and we think this favours mutations that further promote stem cell growth rather than disease.
“Our sample size is quite modest, so we can’t say that blood donation definitely decreases the incidence of pre-leukaemic mutations and we will need to look at these results in much larger numbers of people. It might be that people who donate blood are more likely to be healthy if they’re eligible, and this is also reflected in their blood cell clones. But the insight it has given us into different populations of mutations and their effects is fascinating.”
Hector Huerga Encabo, postdoctoral fellow in the Haematopoietic Stem Cell Laboratory at the Crick, and first joint author with Darja Karpova from the DKFZ in Heidelberg, said: “We know more about preleukaemic mutations because we can see them when people are diagnosed with blood cancer.
“We had to look at a very specific group of people to spot subtle genetic differences which might actually be beneficial in the long-term. We’re now aiming to work out how these different types of mutations play a role in developing leukaemia or not, and whether they can be targeted therapeutically.”
Source: The Francis Crick Institute