Shrinking Brain Volume may be Reflective of Alzheimer’s Treatment Efficacy
Brain shrinkage observed in people receiving drugs for Alzheimer’s treatment actually reflects their efficacy, suggests to a new study from University College London. The researchers analysed data from a dozen different trials of amyloid-targeting immunotherapy – including lecanemab, recently approved in the UK for Alzheimer’s treatment but not yet used by the NHS.
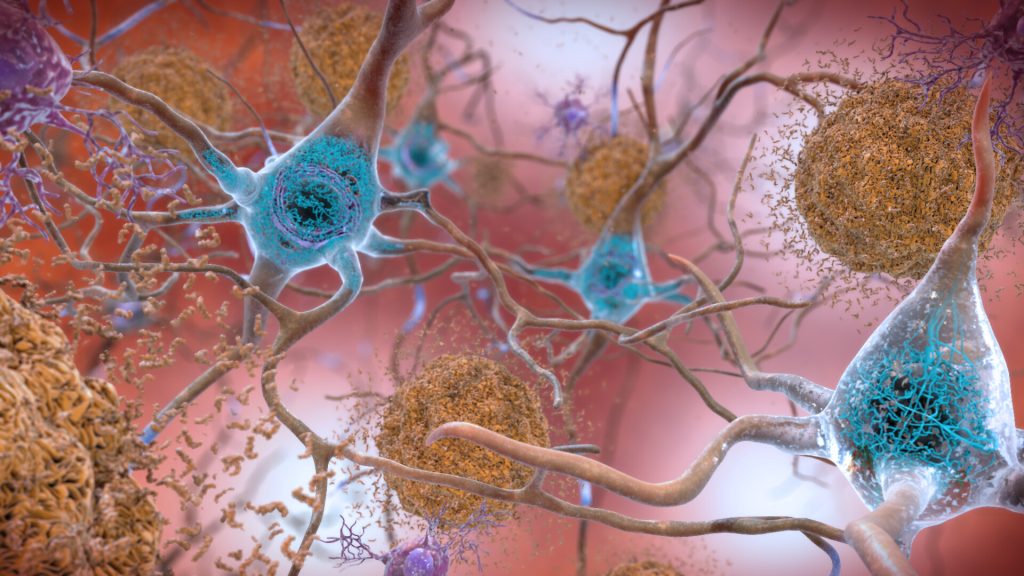
While brain shrinkage is usually an undesirable outcome, the team found that the excess volume loss was consistent across studies and correlated with how effective the therapy was in removing amyloid and was not associated with harm.
As a result, the researchers believe that the removal of amyloid plaques, which are abundant in Alzheimer’s patients, could account for the observed brain volume changes. And, as such, the volume loss should not be a cause for concern.
To describe this phenomenon, the research team coined a new phrase: “amyloid-removal-related pseudo-atrophy” or ARPA. The team published their findings in published in Lancet Neurology.
Senior author and Director of the UCL Dementia Research Centre, Professor Nick Fox said: “Amyloid-targeting monoclonal antibodies represent a significant therapeutic breakthrough in the treatment of Alzheimer’s disease. These agents work by binding to and triggering the removal of amyloid plaques from the brain.
“One area of controversy has been the effect of these agents on brain volumes. Brain volume loss is a characteristic feature of Alzheimer’s disease, caused by progressive loss of neurons.
“Amyloid immunotherapy has consistently shown an increase in brain volume loss – leading to concerns in the media and medical literature that these drugs could be causing unrecognised toxicity to the brains of treated patients.
“However, based on the available data, we believe that this excess volume change is an anticipated consequence of the removal of pathologic amyloid plaques from the brain of patients with Alzheimer’s disease.”
In August, the Medicines and Healthcare Products Regulatory Agency (MHRA) licensed lecanemab, for use in the early stages of Alzheimer’s disease in the UK *.
The drug works by targeting beta amyloid – a protein that builds up in the brains of people with Alzheimer’s disease and is thought to be the triggering event leading to neuronal dysfunction and cell death.
The National Institute for Health and Care Excellence (NICE) that decide whether drugs should be made available on the NHS have published draft guidance advising that the benefits of lecanemab are too small to justify the cost to the NHS. However, the decision will be reviewed following a public consultation and a second independent committee meeting later this year.
Source: University College London