Blood Test for Alzheimer’s Proves Highly Accurate
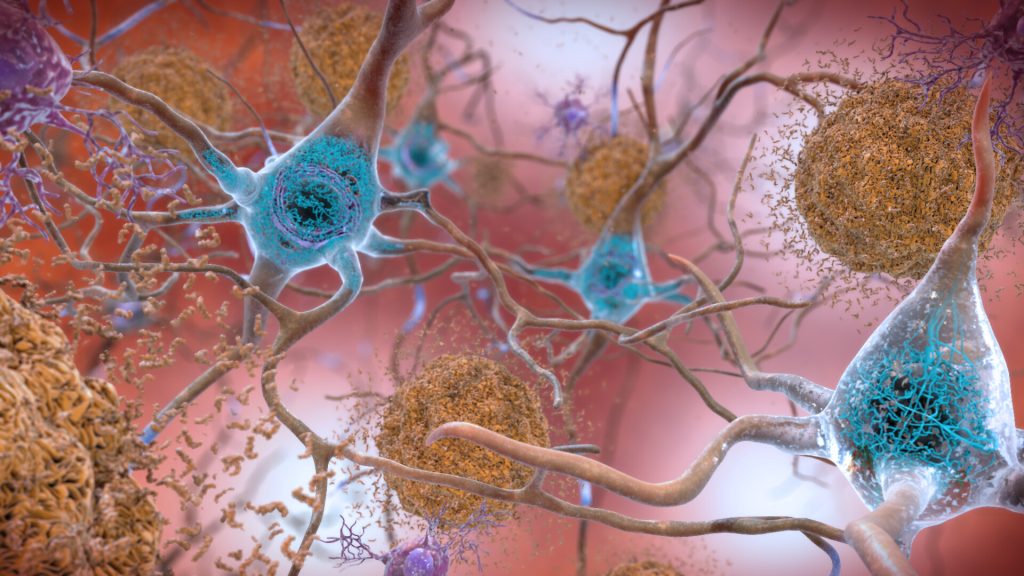
A study in the journal Neurology has shown that a less expensive blood test to detect Alzheimer’s is highly accurate at early detection, providing further evidence that the test should be considered for routine screening and diagnosis.
“Our study shows that the blood test provides a robust measure for detecting amyloid plaques associated with Alzheimer’s disease, even among patients not yet experiencing cognitive declines,” said senior author Professor Randall J. Bateman, MD.
“A blood test for Alzheimer’s provides a huge boost for Alzheimer’s research and diagnosis, drastically cutting the time and cost of identifying patients for clinical trials and spurring the development of new treatment options,” Prof Bateman said. “As new drugs become available, a blood test could determine who might benefit from treatment, including those at very early stages of the disease.”
Developed by Prof Bateman and colleagues, the blood test assesses whether amyloid plaques have begun accumulating in the brain based on the ratio of the levels of the amyloid beta proteins Aβ42 and Aβ40 in the blood.
The gold standard PET scan evaluation requires a radioactive brain scan, at an average cost of $5000–$8000 (R75 000–R120 000) per scan. Another common test, which analyses levels of amyloid-beta and tau protein in cerebrospinal fluid, costs about $1000 (R15 000) but requires a spinal tap process.
This study estimates that prescreening with a $500 (R7500) blood test could halve both the cost and the time it takes to enrol patients in clinical trials that use PET scans. Using only blood testing for screening could be done in under six months, a tenth or less of the cost. The test is currently only available in the US and Europe.
The current study shows that the blood test remains highly accurate, even when performed in different labs following different protocols, and in different cohorts across three continents.
Scientists didn’t know if small differences in sampling methods (such as anticoagulant use) could have a big impact on test accuracy because results are based on subtle shifts in amyloid beta protein levels in the blood. Subtle interfernece in these amyloid protein ratios could have triggered a false negative or positive result.
To confirm the test’s accuracy, researchers tested blood samples from current Alzheimer’s studies in the United States, Australia and Sweden, each of which uses different protocols for the processing of blood samples and related brain imaging.
Findings from this study confirmed that the Aβ42/Aβ40 blood test using a high-precision immunoprecipitation mass spectrometry technique developed at Washington University provides highly accurate and consistent results for both cognitively impaired and unimpaired individuals across all three studies.
When blood amyloid levels were combined with another major Alzheimer’s risk factor – the presence of the genetic variant APOE4 – the blood test accuracy was 88% compared to brain imaging and 93% when compared to spinal tap.
“These results suggest the test can be useful in identifying nonimpaired patients who may be at risk for future dementia, offering them the opportunity to get enrolled in clinical trials when early intervention has the potential to do the most good,” Prof Bateman said. “A negative test result also could help doctors rule out Alzheimer’s in patients whose impairments may be related to some other health issue, disease or medication.”