Improving Prediction of Worsening Knee Osteoarthritis with an AI-assisted Model
New model that combines MRI, biochemical, and clinical information shows potential to enhance care
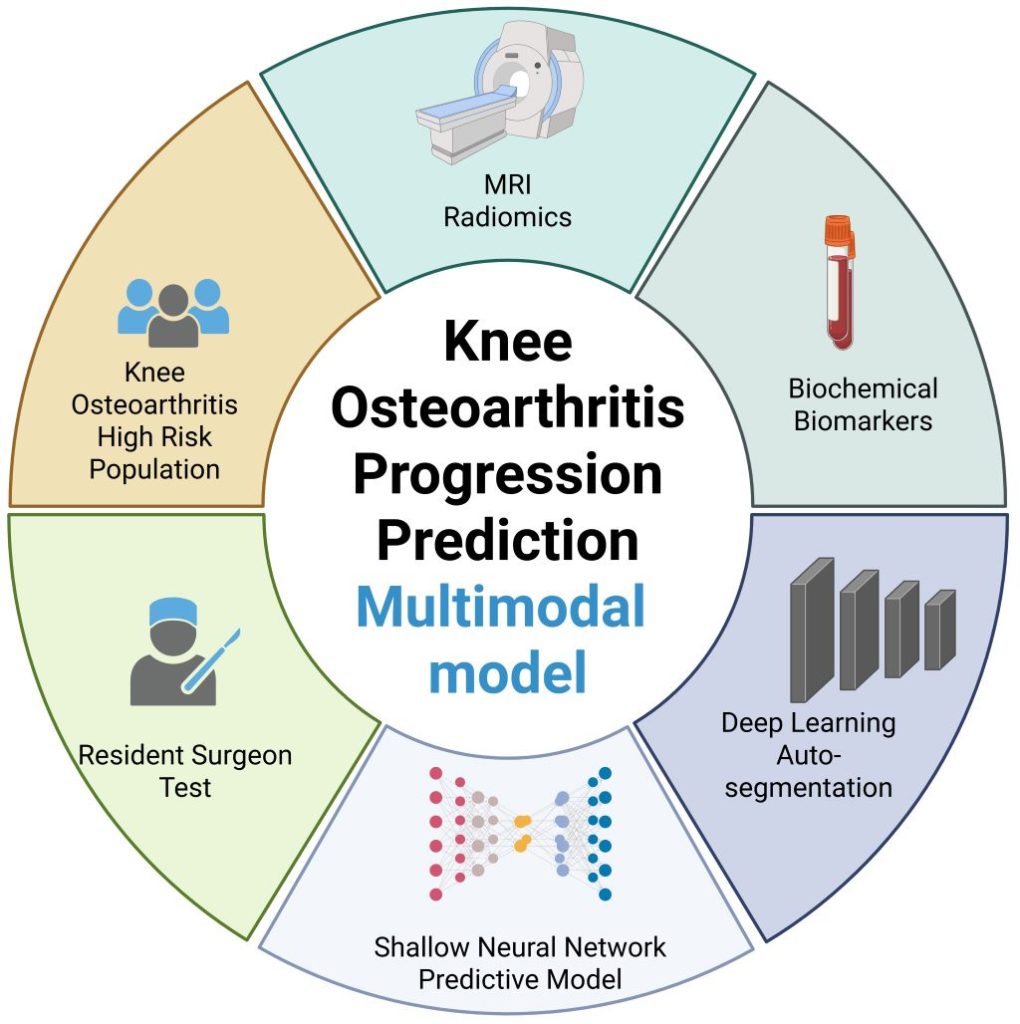
Image credit: Wang T, et al., 2025, PLOS Medicine, CC-BY 4.0
An artificial intelligence (AI)-assisted model that combines a patient’s MRI, biochemical, and clinical information shows preliminary promise in improving predictions of whether their knee osteoarthritis may soon worsen. Ting Wang of Chongqing Medical University, China, and colleagues present this model August 21st in the open-access journal PLOS Medicine.
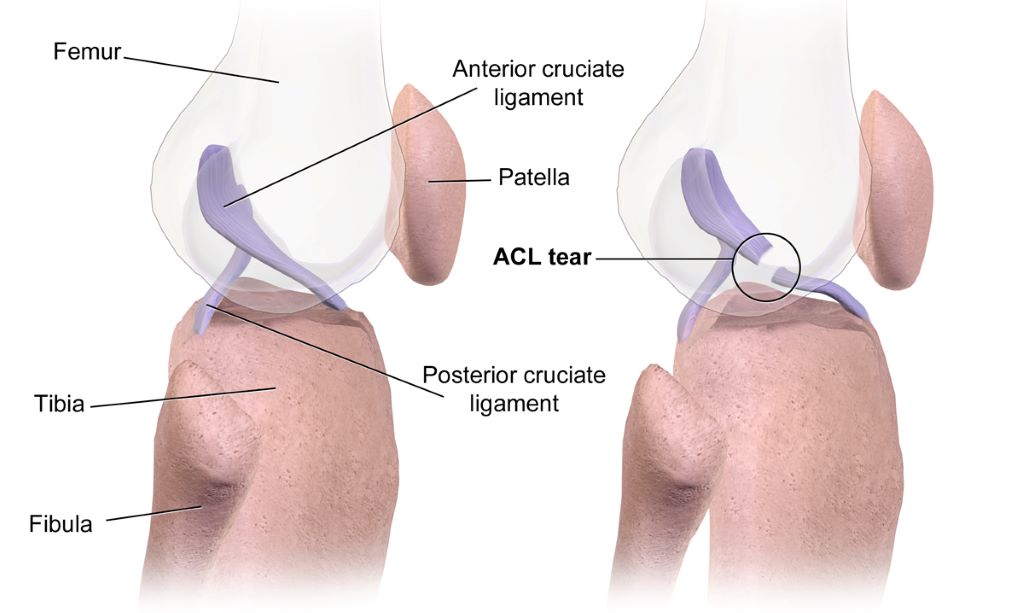
In knee osteoarthritis, cartilage in the knee joint gradually wears away, causing pain and stiffness. It affects an estimated 303.1 million people worldwide and can lead to the need for total knee replacement. Being able to better predict how a person’s knee osteoarthritis may worsen in the near future could help inform more timely treatment. Prior research suggests that computational models combining multiple types of data – including a patient’s MRI results, clinical assessments, and blood and urine biochemical tests – could enhance such predictions.
The integration of all three types of information in a single predictive model has not been widely reported. To address that gap, Wang and colleagues utilized data from the Foundation of the National Institutes of Health Osteoarthritis Biomarkers Consortium on 594 people with knee osteoarthritis, including their biochemical test results, clinical data, and a total of 1,753 knee MRIs captured over a 2-year timespan.
With the help of AI tools, the researchers used half of the data to develop a predictive model combining all three data types. Then, they used the other half of the data to test the model, which they named the Load-Bearing Tissue Radiomic plus Biochemical biomarker and Clinical variable Model (LBTRBC-M).
In the tests, the LBTRBC-M showed good accuracy in using a patient’s MRI, biochemical and clinical data to predict whether, within the next two years, they would experience worsening pain alone, worsening pain alongside joint space narrowing in the knee (an indicator of structural worsening), joint space narrowing alone, or no worsening at all.
The researchers also had seven resident physicians use the model to assist their own predictions of worsening knee osteoarthritis, finding that it improved their accuracy from 46.9 to 65.4 percent.
These findings suggest that a model like LBTRBC-M could help enhance knee osteoarthritis care. However, further model refinement and validation in additional groups of patients is needed.
The authors add, “Our study shows that combining deep learning with longitudinal MRI radiomics and biochemical biomarkers significantly improves the prediction of knee osteoarthritis progression—potentially enabling earlier, more personalized intervention.”
The authors state, “This work is the result of years of collaboration across multiple disciplines, and we were especially excited to see how non-invasive imaging biomarkers could be leveraged to support individualized patient care.”
Co-author Prof. Changhai Ding notes, “This study marks a step forward in using artificial intelligence to extract meaningful clinical signals from complex datasets in musculoskeletal health.”
Provided by PLOS