A Gentle Approach Offers New Hope for Inflammatory Lung Diseases
Pulmonary sarcoidosis is a lung disease characterised by granulomas—tiny clumps of immune cells that form in response to inflammation. It’s the most inflammatory of the interstitial lung diseases (ILDs), a family of conditions that all involve some level of inflammation and fibrosis, or scarring, of the lungs. In the U.S., pulmonary sarcoidosis affects around 200 000 patients. The cause is unknown, and no new treatments have been introduced in the past 70 years.
In a paper published in Science Translational Medicine, scientists at Scripps Research and aTyr Pharma characterised a protein, HARSWHEP, that can soothe the inflammation associated with sarcoidosis by regulating white blood cells. Reducing inflammation slows the disease’s progression and results in less scarring. A phase 1b/2a clinical trial of efzofitimod, a therapeutic form of HARSWHEP, showed promising results.
“Taken together, these results validate a new way to approach immune regulation in chronic lung disease,” says Paul Schimmel, professor of molecular medicine and chemistry at Scripps Research and the study’s senior author.
The drug’s power lies in its gentle nature. “It’s not a hammer; it’s not overly suppressing the immune system. It’s just nudging the immune system in a certain way,” explains Leslie A. Nangle, Vice President of Research at aTyr Pharma and the paper’s first author. “And if you can quiet the inflammation, you can stop the cycle of ongoing fibrosis.”
HARSWHEP is part of an ancient class of proteins known as aminoacyl-tRNA synthetases (aaRSs). Typically, aaRSs play a key role in protein synthesis. “They’re in every cell in your body. They’re in every organism on the planet,” Nangle says. Over time, new versions known as splice variants have emerged that bind to receptors on the outsides of cells and initiate different events throughout the body.
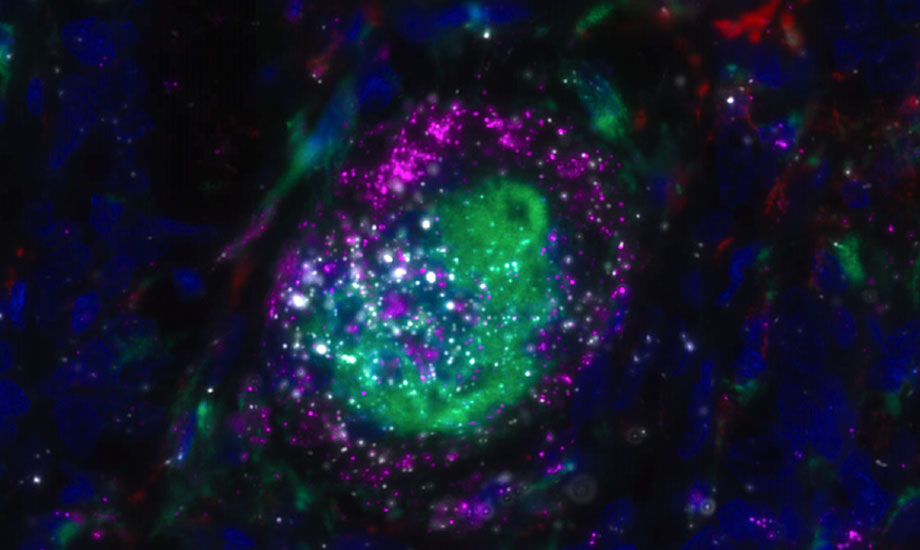
One such variant, HARSWHEP, entered the picture about 525 million years ago. Nangle and Schimmel screened more than 4,500 receptors and were surprised to find that HARSWHEP will bind only to the receptor neuropilin-2 (NRP2). This receptor is known for its role in development of the lymphatic system—the circulatory system through which immune cells travel—not immune function. But the researchers found that when small, circulating white blood cells known as monocytes enter a tissue in response to inflammation and develop into larger, more specialized white blood cells known as macrophages, those cells start to express high levels of NRP2.
“We had a protein with an unknown function. We had a receptor that was doing something on immune cells that had never been characterized. So we had a couple things we had to match up,” Nangle says.
The team found that HARSWHEP binding to NRP2 physically transforms the macrophage. “It’s creating a new type of macrophage that is less inflammatory and actually helps to resolve inflammation,” Nangle explains.
To characterise HARSWHEP’s mechanism of action, the team administered the protein in mice and rats and found that it reduced lung inflammation and the progression of fibrosis.
In separately published clinical trial data, the team saw a positive impact on patients who were treated with efzofitimod while tapering off of oral corticosteroids. Long-term steroid treatment, currently the first-line option, is associated with significant weight gain and organ damage, and the immunosuppressive effects leave patients vulnerable to infection.
The team also characterised patients’ circulating immune cells before and after efzofitimod treatment. They saw that it reduced key indicators of the inflammation that drives sarcoidosis, such as the concentration of macrophages and other inflammatory immune cells.
While they’re exploring sarcoidosis first, efzofitimod is a potential treatment for many interstitial lung diseases, Nangle explains. The aTyr team plans to explore treating other ILDs and is running a clinical trial now for scleroderma-related ILD.
The work highlights macrophages as a possible target for treating ILDs, and the promise of HARSWHEP could foretell other aaRSs’ therapeutic potential.
Nangle describes this work as moving “from concept to clinic.” Schimmel has worked on aaRSs throughout his tenure at Scripps Research. aTyr Pharma spun out of Schimmel’s lab; his former graduate student Nangle was the company’s first employee upon opening their labs in 2006.
“Original work that happened at Scripps gave rise to the idea that this could be a new class of therapeutic molecules, Nangle says. “We have now moved it all the way to clinical development. It’s a proof of concept for this whole class of molecules and the work Paul has done.”
Source: Scripps Research Institute