A New Insight into the Mechanisms of Epidermal Renewal
The mechanisms underlying skin renewal are still poorly understood, but interleukin-38 (IL-38), a protein involved in regulating inflammatory responses, could provide insights. Researchers observed it for the first time in the form of condensates in keratinocytes, the cells of the epidermis. The presence of IL-38 in these aggregates is enhanced close to the skin’s surface exposed to atmospheric oxygen. This process could be linked to the initiation of programmed keratinocyte death, a natural process in the epidermis. This study, from University of Geneva (UNIGE) researchers, could bring new perspectives for the study of human epidermis and the illnesses that affect it.
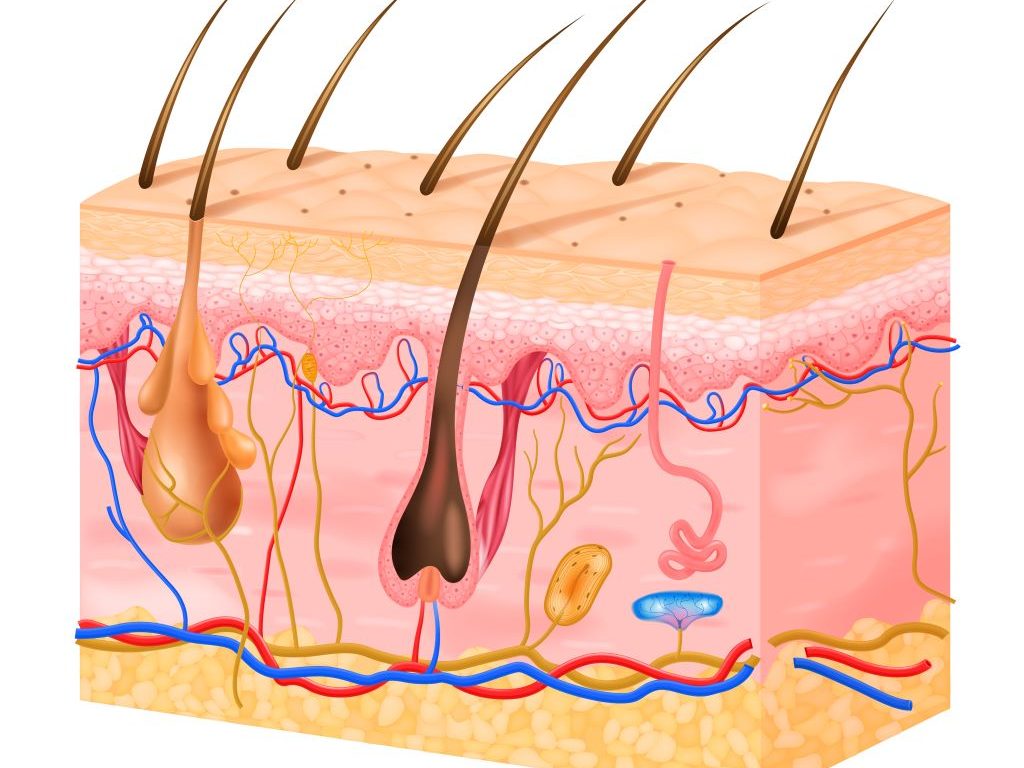
Renewal of the epidermis relies on stem cells located in its lowest layer, which constantly produce new keratinocytes. These new cells are then pushed to the surface, differentiating along the way and accumulating protein condensates. Once they reach the top of the epidermis, they undergo a programmed death, cornification, to create a protective barrier of dead cells.
“The way in which the epidermis constantly renews itself is well documented. However, the mechanisms that drive this process are still not fully understood,” explains Gaby Palmer-Lourenço, associate professor at the Faculty of medicine of UNIGE and principal investigator. The study is published in the journal Cell Reports.
An unexpected role
Interleukin 38 is a small messenger protein that ensures communication between cells. It is known for its role in regulating inflammatory responses and its presence in keratinocytes, the cells of the epidermis, was previously associated with the preservation of the skin’s immune balance. “In keratinocytes in vivo, we found that IL-38 forms condensates, specialized protein aggregates with specific biochemical functions, a behavior that was not known for this protein,” recounts Gaby Palmer-Lourenço. Even more curious, the closer the keratinocytes were to the surface of the skin, the greater the amount of IL-38 within these condensates.
A reaction to oxidative stress
Blood vessels stop in the skin layer located below the epidermis. Therefore, the quantity of oxygen available for the keratinocytes is lower in the basal layers of the epidermis compared to the top layers that are directly exposed to the air that surrounds us. However, even though it is necessary to maintain cell functions, oxygen also causes oxidative stress by forming free radicals, reactive molecules that endanger the cell. “We were able to show that oxidative stress does indeed cause IL-38 condensation under laboratory conditions,” confirms Alejandro Díaz-Barreiro, postdoctoral fellow at the UNIGE Faculty of medicine, and first author of the study.
“Our results lead us to believe that, as we move closer to the epidermal surface, the increasing oxygen concentration promotes the formation of protein condensates, indicating to keratinocytes that they are in the right place to enter cell death,” furthers Gaby Palmer-Lourenço. This hypothesis provides new leads to decipher the mechanisms of epidermal renewal. It could also pave the way for a better understanding of the pathological mechanisms underlying certain skin diseases, such as psoriasis or atopic dermatitis. These questions will be further examined by the research group in future studies.
Contributing to an alternative to animal models
Alejandro Díaz-Barreiro is already working on the next step: “In the model we used previously, the effects of oxidative stress were artificially induced in a single layer of keratinocytes, a scenario that differs from the actual situation in the skin. We are therefore developing a new experimental system to apply oxygen gradients to in vitro reconstituted human epidermis. In this model, only the skin surface will be exposed to ambient air, while the other layers will be protected. This will allow us to study in detail the effect of oxidative stress on epidermal renewal.” By enabling a more precise analysis of human cells, this new system will provide an alternative to animal models often used for the study of skin biology and disease.
Source: Université de Genève