Ventilation in Hospitals could Actually Spread Viruses Further

Increased use of ventilation and air cleaners, designed to mitigate the spread of viral infections in hospitals, is likely to have unpredictable effects and may cause viral particles to move around more, according to a new study from researchers at UCL and UCLH.
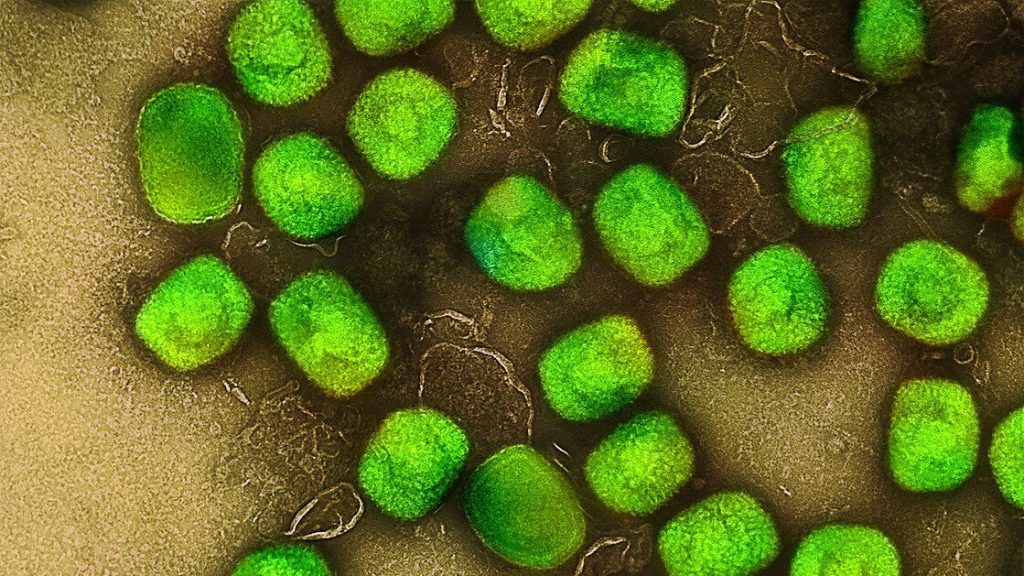
In the study, published in Aerosol Science & Technology, researchers investigated the effect of using built-in mechanical ventilation and portable air cleaners (PACs)1 upon the spread of airborne particles, which are similar to those breathed out by a person with a viral respiratory infection such as SARS-CoV-2 or influenza.
The team tracked the movement of airborne particles around a typical hospital outpatients’ clinic at UCLH in central London using an aerosol generator and particle counters2. A variety of scenarios were simulated, including particle movement to a neighbouring room, throughout the whole clinic, and from one room to another room at the far side of the clinic.

They also tested whether factors such as closing doors, or the position of ventilation and PACs within a room, had an effect on the spread of particles.
The researchers found that while use of built-in ventilation and PACs can reduce particle spread in some scenarios, in some experiments the use of PACs increased aerosol spread by up to 29% between neighbouring rooms. Built-in ventilation potentially increased aerosol migration across the clinic by up to 5.5 times more than if no ventilation was used.
Professor Laurence Lovat, senior author of the study from UCL Surgery & Interventional Science and UCLH, said: “The COVID-19 pandemic really highlighted the risk of picking up airborne viral infections in hospitals, which naturally led to efforts to reduce this risk. In many hospitals, the use of ventilation systems and portable air cleaners has increased.
“While the urgency of the situation demanded a rapid response, since then we’ve been studying precisely how viral particles move around in real spaces and have been surprised by what we’ve found.
“Putting air cleaners in rooms led to unexpected increases in the circulation of aerosols in some cases, but it took months to understand what we were seeing. Each scenario produced different, unexpected results, depending on the spaces and airflow sources involved.
“Even at UCLH, a modern hospital built less than 20 years ago, airflow patterns were not predictable. In older hospitals, which often have natural draughts, the situation would likely be even more complex.”

The study concluded that using airflow devices in hospitals to try to limit the movement of airborne pathogens requires careful consideration of airflow dynamics and device placement to reduce the risk of exacerbating the problem.
The clinic where the experiments took place consisted of a large central waiting room (154 m3,split into A and B for the purpose of the study), eight surrounding consulting rooms and a nurses’ station (all approximately 35 m3). The clinic was connected via a permanently open passageway to a corridor leading to the rest of the hospital. Experiments took place at night and weekends when no staff or patients were present.
A number of experiments were conducted by placing aerosol generators dispersing saline solution in certain rooms, with particle detectors sited in other rooms to track the movement of particles around the clinic.
In one experiment, the researchers simulated particle spread from a medical professional or patient in one consulting room to a neighbouring room. A baseline measurement was taken in the consulting room with the aerosol source when all doors were open and no ventilation or PACs were in use.
Closing the room door that contained the source was found to reduce particle spread significantly and closing both room doors reduced it by 97%.
But when doors were opened and large PACs in the adjacent waiting room were turned on, the spread to the neighbouring consulting room increased by 29%. When small desktop PACs were added to both consulting rooms and the nurses’ station, the spread was lower than the baseline, but only slightly.
Dr Jacob Salmonsmith, first author of the study and an Honorary Research Fellow from UCL Mechanical Engineering, said: “The results of this experiment might seem counterintuitive if you take the view that changing the air in a room more often reduces the spread of viral particles.
“While it’s true that air cleaners do remove viral particles from the air and can reduce overall spread, they can also have unintended consequences. In particular, this experiment suggests that larger air cleaners, which have larger exhaust vents that introduce their own air currents, can cause particles that haven’t been filtered out to spread further than they would have if the cleaner wasn’t there.
“In any given space you have complex interactions between many different air currents, such as ventilation, doors closing and people’s movement. Our findings indicate that the whole picture needs to be considered when choosing when and where to introduce air cleaners.”
In another experiment, the team observed highly complex patterns of particle spread when all consulting room doors were open.
This included one scenario where the highest concentrations of particles were detected in rooms furthest away from an aerosol source situated in a consulting room where a PAC was in operation. Particle levels in the room furthest from this aerosol source were 184% higher than average, while in the room directly opposite the source they were 68% below average.
There were also 247% more particles in the waiting room furthest away from the consulting room, where a PAC was in operation, than in the waiting room right next door to it. The nurses’ station had a higher concentration of particles than any room on the same side of the clinic as the room where the aerosol generator was situated.
Professor Andrea Ducci, an author of the study from UCL Mechanical Engineering, said: “Our experiments demonstrated that high volume of particles can be corralled into particular areas as a result of airflow dynamics. This obviously isn’t ideal, particularly if that place is a key location, such as the nurses’ station that staff members who’re treating patients will likely visit often during their shift.
“The good news is that we’re rapidly expanding our knowledge of this phenomenon. The project that we are currently working on aims to simulate the entire airflow within a clinic and assess the efficacy of different devices positioned in different locations. This will allow us to identify relatively simple interventions, such as better positioning of ventilation devices to reduce the spread of particles, thus decreasing the risk of picking up an infection in hospital.”
Given the unpredictability of how aerosol particles move around spaces and the difficulty in measuring them, the team are currently building an AI system to help to do this and hope to start testing within the next 18 months.
The authors say the study holds great promise to inform governmental action on ensuring that NHS standards for ventilation and infection are fit for purpose, in line with efforts to prevent future pandemics.
1 Portable air cleaners, or purifiers, are devices that filter dust and fine particles out of the air. The devices used in this study all conformed to the HEPA standard, meaning they are designed to filter out almost all (99.7%) of the fine particles that pass through them. The PACs placed in the waiting room were large (around the size of a kitchen bin) and the ones used in smaller room were around the size of a desktop lamp.
2 The aerosol particles were created from a harmless saline solution and disbursed at a constant rate by an aerosol generator at roughly the face height of a seated person (1.2 metres). The particles were designed to mimic those breathed out by a person with an airborne respiratory infection, such as influenza.
Source: University College London