Unleashing the Immune System to Attack Cancers
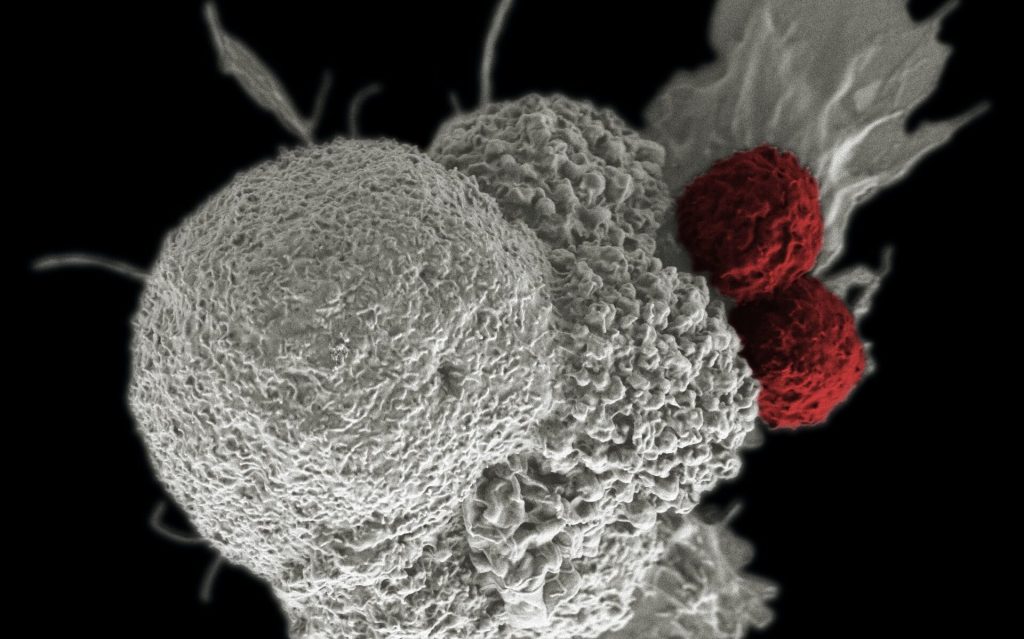
A potential treatment has been identified, that could boost the immune system’s ability to find and destroy cancer cells, by impeding certain cells which regulate the immune system, which in turn can unleash other immune cells to attack tumours in cancer patients.
“A patient’s immune system is more than able to detect and remove cancer cells and immunotherapy has recently emerged as a novel therapy for many different types of cancers,” explained study leader Nullin Divecha, Professor of Cell Signalling at the University of Southampton. “However, cancer cells can generate a microenvironment within the tumour that stops the immune system from working thereby limiting the general use and success of immunotherapy,” he continued.
One of a number of types of T cells, Teffector cells (Teffs) carry out the task of detection and removal of cancer cells . How well Teff cells work in detecting and removing cancer cells is partly governed by other T cells called T-regulatory cells, or Tregs for short. Tregs physically interact with the Teff cells, producing molecules which dampen the functioning of the Teff cells.
Prof Divecha added, “Tregs carry out an important function in the human body because without them, the immune system can run out of control and attack normal cells of the body. However, in cancer patients we need to give the Teff cells more freedom to carry out their job.”
Molecules released by tumour cells exacerbate the problem by attracting and gathering Tregs, reducing the activity and function of Teff cells even further. Though there are mechanisms to inhibit Treg cells, since Treg and Teff cells are very similar, Teff cells are also generally inhibited.
In this new study, published in PNAS, scientists from the University of Southampton and the National Institute of Molecular Genetics in Milan showed that inhibition of a family of enzymes in cells called PIP4K could be the answer to how to restrict Tregs without affecting Teffs.
The research team isolated Tregs from healthy donors and used genetic technology to suppress the production of the PIP4K proteins. They saw that loss of PIP4Ks from Treg cells stopped their growth and response to immune signals, in turn stopping them from impeding Teff cell growth and function.
Importantly, the loss of the same enzymes in Teff cells did not limit their activity.
“This was surprising because PIP4Ks are in both types of T cells in similar concentrations but our study shows that they seem to have a more important function for Tregs than Teffectors,” said Dr. Alessandro Poli who carried out the experimental research.
Scientists must next develop molecules in order to inhibition of PIP4K as a potential therapy for patients. “Towards this end we show that treatment with a drug like inhibitor of PIP4K could enable the immune system to function more strongly and be better equipped to destroy tumour cells.”
Source: EurekAlert!