How Checkpoint Immunotherapy also Increases the Risk of Cardiovascular Disease

Cancer immunotherapy is known to also make patients more vulnerable to heart attack and stroke. A new study led by researchers at NYU Langone Health points to a possible explanation for this side effect: the treatment interferes with immune regulation in the heart’s largest blood vessels.
This new work focused on immune checkpoint inhibitors, which work by blocking molecules embedded on the surface of cells – immune checkpoints – which normally serve as “brakes” that prevent excess immune activity, or inflammation. Some tumours are known to hijack these checkpoints to weaken the body’s defences, so by blocking the checkpoints, the treatments enable the immune system to kill tumour cells.
Unfortunately, this treatment type may also trigger damaging levels of inflammation in the heart, brain, stomach, and other organs, the researchers say. For example, past studies have shown that about 10% of those with atherosclerosis have a heart attack or stroke following cancer treatment. Until now, the specific mechanisms behind this issue had remained unclear.
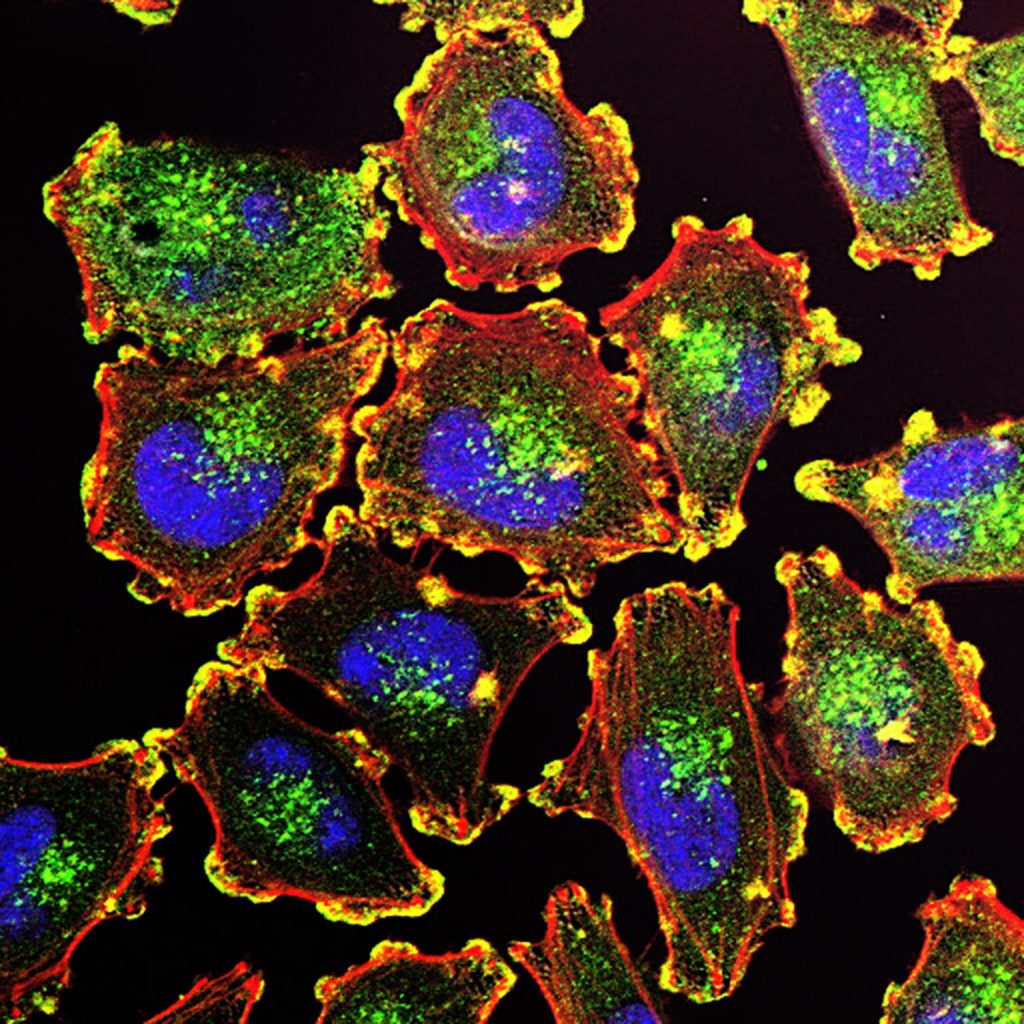
To address this question, the research team explored at a cellular level how immune checkpoint inhibitors interact with immune cells within arterial plaques. A genetic analysis by the study authors showed that the same type of immune checkpoints targeted by cancer therapies also appear in arterial immune cells, establishing a link between checkpoint inhibitors and cardiovascular events.
“Our findings provide new insight into how a drug intended to target tumours can also prompt a heightened immune response in arteries and increase risk of heart disease,” said study co-senior author Chiara Giannarelli, MD, PhD. “Cancer patients and their physicians should be aware that they may need to monitor for new heart concerns following cancer treatment,” added Dr Giannarelli.
For the current study, published in Nature Cardiovascular Research, the researchers analysed the genetic activity of thousands of immune cells collected from the plaques of 50 men and women undergoing a surgical procedure to address atherosclerosis.
The investigators also explored how type 2 diabetes, a known risk factor for both cancer and heart disease, may make those with atherosclerosis even more vulnerable to the ill effects of checkpoint inhibitors, adds Dr Giannarelli, also an associate professor in the Department of Pathology at NYU Grossman School of Medicine. As part of the study, the team assessed immune checkpoint activity in arterial tissue collected from eight patients with diabetes and four healthy volunteers. Notably, none had a history of atherosclerosis. The results showed that the diabetes patients had less measurable communication between checkpoints, which in turn can prompt increased inflammation.
Other experiments further revealed that taking immune checkpoint inhibitors might make it harder to combat atherosclerosis. Under normal circumstances, physicians typically prescribe low-fat diets to reduce plaque buildup and inflammation. Indeed, the researchers’ experiments in rodents confirmed that such diets boost communication between immune checkpoints within arteries. However, cancer patients may be at a disadvantage because their therapy, by blocking these same checkpoints, may counteract the anti-inflammatory benefits of fat reduction.
“Our findings highlight how cancer, diabetes, and heart disease do not exist in a vacuum, and that it is critical to consider how targeting one of these conditions can affect the others,” said study co-senior author Kathryn J. Moore, PhD. “Now that experts have a better understanding of the interplay between these diseases, they can begin to explore new strategies to lower the risk of unintended health concerns caused by their treatment,” added Dr Moore. She cautions that the study did not directly assess immune checkpoint behaviour in cancer patients. The team plans to do so in future investigations, she adds.
Source: NYU Langone Health