More Physical Activity Linked to Fewer Respiratory Infections in Children

A study of 104 children wearing pedometers to monitor daily activity showed that higher levels of physical activity are associated with reduced susceptibility to upper respiratory tract infections such as the common cold. Reporting the findings in Pediatric Research, the researchers suggest reduced inflammatory cytokines and improved immune responses as a possible mechanism.
Wojciech Feleszko, Katarzyna Ostrzyżek-Przeździecka and colleagues measured the physical activity levels and symptoms of upper respiratory tract infections of children aged between four and seven years in the Warsaw city region between 2018 and 2019. Participants wore a pedometer armband 24 hours a day for 40 days to measure their activity levels and sleep duration. For 60 days, parents used daily questionnaires to report their children’s symptoms of upper respiratory tract infections, such as coughing or sneezing. On a second questionnaire, parents reported their children’s vaccinations, participation in sport, whether they had siblings, and their exposure to smoking and pet hair.
The authors found that as the average daily number of steps taken by children throughout the study period increased by 1000, the number of days that they experienced symptoms of upper respiratory tract infections decreased by an average of 4.1 days. Additionally, children participating in three or more hours of sport per week tended to experience fewer days with respiratory tract infection symptoms than those not regularly participating in sports.
Higher activity levels at the beginning of the study were associated with fewer days with respiratory tract infection symptoms during the following six weeks. Among 47 children, with 5668 average daily steps during the first two weeks of the study period, the combined number of days during the following six weeks that these children experienced upper respiratory tract infection symptoms was 947. However, among 47 children whose initial average daily steps numbered 9368, the combined number of days during the following six weeks that these children experienced respiratory symptoms for was 724. Upper respiratory tract infection symptoms were not associated with sleep duration, siblings, vaccinations, or exposure to pet hair or smoking.
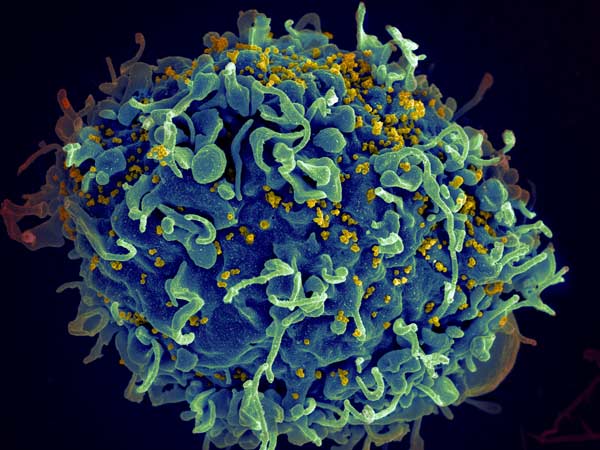
The authors speculate that higher physical activity levels could help reduce infection risk in children by reducing levels of inflammatory cytokines and by promoting immune responses involving T-helper cells. They also suggest that skeletal muscles could release small extracellular vesicles that modulate immune responses following exercise. However, they caution that future research is needed to investigate these potential mechanisms in children. In addition, since this was an observational study, causality could not be established.
Source: EurekAlert!