Inflammation may Explain the Prevalence of IBD in Psoriasis Sufferers

People with psoriasis often have invisible inflammation in the small intestine with an increased propensity for ‘leaky gut’, according to new research at Uppsala University. These changes in the gut could explain why psoriasis sufferers often have gastrointestinal problems and are more prone to developing Crohn’s disease. The study is published in Biochimica et Biophysica Acta (BBA) – Molecular Basis of Disease.
Psoriasis is a hereditary, chronic skin condition that can also result in inflammation of the joints. Chronic inflammatory bowel diseases (IBD), especially Crohn’s disease, are more common in patients with psoriasis than in the rest of the population.
“Previous research has also shown that people with psoriasis have more gastrointestinal problems than the general population. However we didn’t know much about why this is the case. With our study, we can now show that people with psoriasis often have invisible inflammation in their small intestines, with an increased risk of what’s called leaky gut,” says Maria Lampinen, researcher at Uppsala University.
Pro-inflammatory activity in the gut
The study involved 18 patients with psoriasis and 15 healthy controls as subjects. None of the participants had been diagnosed with gastrointestinal diseases. Samples were taken from both their small and large bowel. The researchers then studied different types of immune cells in the mucous membrane.
“It turned out that psoriasis sufferers had higher numbers of certain types of immune cells in their small intestine, and the cells showed signs of pro-inflammatory activity. Interestingly, we found the same type of immune cells in skin flare-ups from psoriasis patients, suggesting that the inflammation of the skin may have an impact on the gut, or vice versa.
Increased propensity for leaky gut
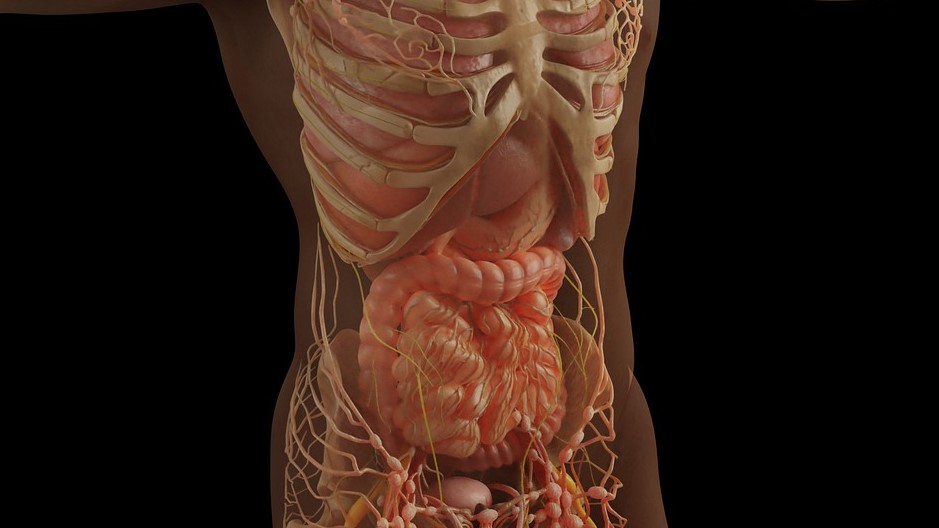
Normally, the intestinal mucosa act as a protective barrier that also allows nutrients and water to pass through it. In some autoimmune diseases, the intestinal barrier may function poorly. This is called having a leaky gut, and leads to bacteria and harmful substances leaking through the intestinal barrier and causing inflammation. This can also cause more widespread inflammation when these substances are spread via the bloodstream.
Half of the psoriasis patients in the study had increased intestinal barrier permeability or leaky gut. These same patients also reported more gastrointestinal symptoms such as abdominal pain and bloating than patients with a normal intestinal barrier. They also had elevated levels of inflammatory substances in their intestines.
“Given that the psoriasis patients in our study had relatively mild skin disease and showed no visible intestinal inflammation in a gastroscopy, they had surprisingly clear changes in their small intestine compared to healthy controls. These changes could explain why psoriasis sufferers often have gastrointestinal problems, and an increased risk of developing Crohn’s disease.
Source: Uppsala University