‘One-dose’ Course Effective for HIV-associated Cryptococcal Meningitis
A new short course of treatment for HIV-associated cryptococcal meningitis is as effective as the longer, standard one, and is better tolerated, according to a real-world study in the New England Journal of Medicine.
The international study involved a randomised trial in southern and eastern Africa. This new ‘one-dose’ approach offers a practical, easier-to-administer and better tolerated treatment for HIV-associated cryptococcal meningitis in Africa, the researchers said.
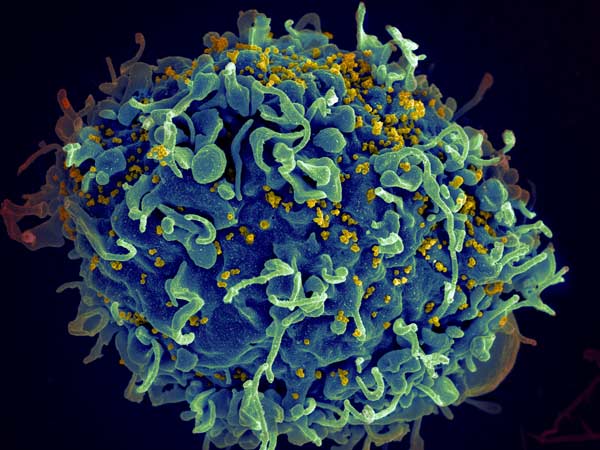
Cryptococcal meningitis causes a serious disease in immunosuppressed people living with HIV, with around 180 000 cryptococcal meningitis-related deaths each year, mostly in sub-Saharan Africa. Current treatments are either a 7 or 14-day course of amphotericin-B, combined with either oral antifungal tablets or oral fluconazole.
This new trial investigated whether a single high dose of liposomal amphotericin-B (L-AmB, Ambisome) paired with two oral antifungals, fluconazole and flucytosine, was as effective at reducing deaths as the currently recommended WHO first-line treatment based on seven days of Amphotericin-B therapy.
Dr Melanie Alufandika-Moyo, study author and the lead research doctor at the Malawi-Liverpool Wellcome Unit, said: “Cryptococcal meningitis is the most common type of adult meningitis in much of Africa. Without effective treatment, infection progresses quickly, often resulting in deaths. Current treatment requires prolonged hospitalisation, intensive nursing care and costly laboratory monitoring which can be expensive for the healthcare system and the patient. Amphotericin-B can also cause kidney damage and blood problems.
“We urgently need new ways of treating the disease, so it’s fantastic that we were able to show a new streamlined treatment, requiring just one intravenous infusion, is as effective and less dangerous for patients.”
More than 800 adult patients with a first episode of HIV-associated cryptococcal meningitis, from five countries in southern and eastern Africa, took part in the trial.
Half received, and half received standard care. After 10 weeks, 25% (101/407) of people in the AmBisome arm died compared to 29% (117/407) in the control arm – this is among the lowest mortality rate reported from a major cryptococcal meningitis trial in Africa, despite more than a quarter of participants presenting with very severe disease.
Drug-related toxicity was significantly lower in the new ‘one-dose’ AmBisome arm. Anaemia occurred in 13% of AmBisome participants compared to 39% in the control arm, with more participants in the control arm needing blood transfusions. Far less drug related kidney toxicity was observed in the one dose AmBisome arm than in the control arm.
AmBisome, a liposomal formulation of amphotericin-B, was suspected to be an effective cryptococcal meningitis treatment as it is less toxic and can be given in large doses that remain in the brain for some time. A single, high-dose of AmBisome had previously been shown to be effective at clearing Cryptococcus from around the brain, which prompted the real-world trial.
Professor Tom Harrison from St George’s, University of London, who co-led the trial with Professor Joe Jarvis from the London School of Hygiene & Tropical Medicine and Botswana Harvard AIDS Institute Partnership, said: “These exciting results represent the culmination of a long programme of collaborative work to optimise antifungal drug combinations and reduce deaths from this terrible infection, and provide the strong evidence needed for policymakers to decide how cryptococcal meningitis should be treated going forward.
“Fortunately, with the support of advocates and funders, Ambisome and flucytosine are now becoming more available, which is essential to enable wide-scale implementation of this novel treatment regimen.”
Professor Joe Jarvis, the lead author of the study, said: “The results of this trial have the potential to transform how cryptococcal meningitis is treated and the management of advanced HIV-related disease in sub-Saharan Africa. It has far fewer significant side effects, which is obviously hugely important, and has the potential to prevent a large number of deaths in low-resource settings by being both easier to administer and cost-effective.”
Study imitations included the current lack of access to Ambisome and flucytosine, the key components of this novel treatment regimen, in many low-resource settings. To address this, an additional five years funding has been received.





