Curing HIV with a Dual Gene Editing Approach

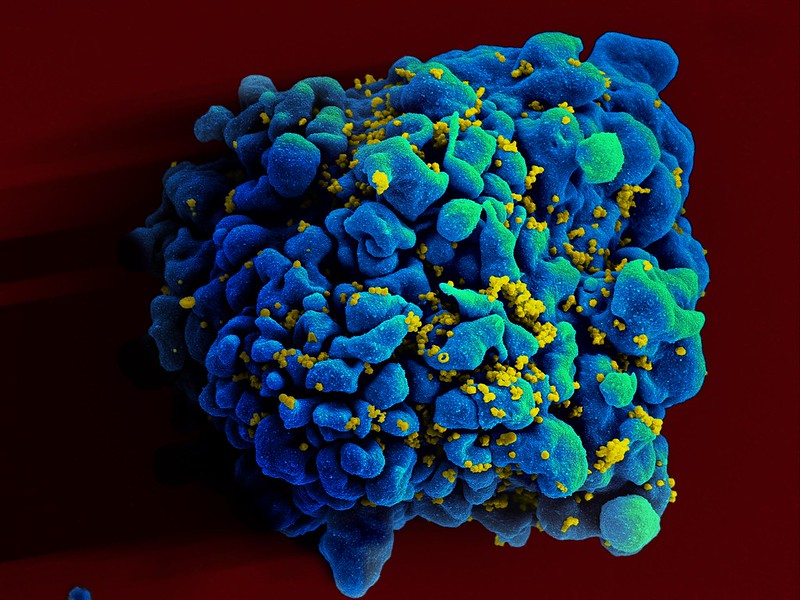
Gene editing therapy aimed at two targets – HIV-1 and CCR5, the co-receptor that helps the virus get into cells – can effectively eliminate HIV infection, report scientists in PNAS. This is the first to combine a dual gene-editing strategy with antiretroviral drugs to cure animals of HIV-1.
“The idea to bring together the excision of HIV-1 DNA with inactivation of CCR5 using gene-editing technology builds on observations from reported cures in human HIV patients,” said Kamel Khalili, PhD, professor at the Lewis Katz School of Medicine. “In the few instances of HIV cures in humans, the patients underwent bone marrow transplantation for leukaemia, and the donor cells that were used carried inactivating CCR5 mutations.”
Dr Khalili and Howard E. Gendelman, MD, professor at UNMC, were senior investigators on the new study from the Lewis Katz School of Medicine at Temple University and the University of Nebraska Medical Center (UNMC). The two researchers have been long-time collaborators and have strategically combined their research strengths to find a cure for HIV.
“We are true partners, and what we achieved here is really spectacular,” Dr Gendelman said. “Dr Khalili’s team generated the essential gene-editing constructs, and we then applied those constructs in our LASER-ART mouse model at Nebraska, figuring out when to administer gene-editing therapy and carrying out analyses to maximise HIV-1 excision, CCR5 inactivation, and suppression of viral growth.”
In previous work, Drs Khalili and Gendelman and their respective teams showed that HIV can be edited out from the genomes of live, humanised HIV-infected mice, leading to a cure in some animals. For that research, CRISPR gene-editing technology for targeting HIV-1 was combined with a therapeutic strategy known as long-acting slow-effective release (LASER) antiretroviral therapy (ART). LASER ART holds HIV replication at low levels for long periods of time, decreasing the frequency of ART administration.
Despite being able to eliminate HIV in LASER-ART mice, the researchers found that HIV could eventually re-emerge from tissue reservoirs and cause rebound infection. This effect is similar to rebound infection in human patients who have been taking ART but suddenly stop or experience a disruption in treatment. HIV integrates its DNA into the genome of host cells, it can lie dormant in tissue reservoirs for long periods of time, out of reach of antiretroviral drugs. As a consequence, when ART is stopped, HIV replication renews, giving rise to AIDS.
To prevent rebound infection, Dr Khalili and colleagues began work on next-generation CRISPR technology for HIV excision, developing a new, dual system aimed at permanently eliminating HIV from the animal model. “From success stories of human HIV patients who have undergone bone marrow transplantation for leukaemia and been cured of HIV, our hypothesis was that the loss of the virus’s receptor, CCR5, is important to permanently eliminating HIV infection,” he explained. They developed a simple and more practical procedure for the inactivation of CCR5 that includes an IV inoculation of the CRISPR gene editing molecule.
Experiments in humanized LASER-ART mice carried out by Dr Gendelman’s team showed that the constructs developed at Temple, when administered together, resulted in viral suppression, restoration of human T-cells, and elimination of replicating HIV-1 in 58% of infected animals. The findings support the idea that CCR5 has a key role in facilitating HIV infection.
The Temple team also anticipates soon testing the dual gene-editing strategy in non-human primates.
The new dual CRISPR gene-editing strategy holds exceptional promise for treating HIV in humans. “It is a simple and relatively inexpensive approach,” Dr Khalili noted. “The type of bone marrow transplant that has brought about cures in humans is reserved for patients who also have leukaemia. It requires multiple rounds of radiation and is not applicable in resource-limited regions, where HIV infection tends to be most common.”
Source: Temple University Health System