US Funding Remains Frozen for Many Life-saving Services
Despite waivers, court judgments and assurances from the embassy, USAID funding for projects that provide HIV medication has not resumed

Numerous South African health projects funded by the US President’s Emergency Plan for AIDS Relief (PEPFAR) remain closed. This is despite a federal court judgment which ordered President Donald Trump’s administration to lift the blanket freeze on global aid.
A waiver on life-saving humanitarian services appears to have had little effect. Funding remains frozen for many projects that provided services explicitly covered by the waiver, such as antiretroviral (ARV) medicines for people with HIV.
A spokesperson for one of these projects said that the United States Agency for International Development Aid (USAID) had not provided any communication regarding the waiver, despite requests for information.
A second organisation said USAID instructed it to provide an adapted budget that only covers services included in the waiver. The organisation submitted it, but it has not yet been approved. The organisation supports orphaned children living with HIV.
CDC funding
PEPFAR is a US initiative that provides billions of dollars a year toward combating HIV in different parts of the world. These funds are primarily distributed through two agencies: USAID and the Centers for Disease Control and Prevention (CDC).
In late January USAID issued stop-work orders to the organisations which it funds. A few days later, the CDC did the same. This was after an executive order by Trump which paused foreign development funding for 90 days pending a review. As a result, US-funded health organisations across South Africa were forced to close their doors. In some cases, HIV patients were left without ARVs.
Last week the CDC issued notifications to its recipient organisations rescinding the stop-work orders. The CDC stated that this was because of a temporary restraining order issued by a federal judge in Rhode Island that halted the Trump administration’s ability to freeze congressional funds. Since then, many South African organisations that get money from the CDC have reopened.
See also: How USAid freeze sent shockwaves through Ethiopia published in The Guardian
But USAID did not send out similar notifications. PEPFAR funds from this agency largely remain frozen.
In a separate judgment on 13 February, a federal judge in Washington DC blocked the implementation of Trump’s executive order to freeze foreign aid. The administration’s lawyers have argued that the US government can continue to freeze aid via other channels unrelated to the executive order.
Dangerous disruption
GroundUp and Spotlight visited three health centres in South Africa funded by USAID, and found all three remained closed. Representatives from a fourth USAID-funded organisation confirmed that its funding has not been restored, and that its partner organisation was in the same boat.
The first centre that we visited is a clinic in Rosebank, Johannesburg, run by OUT LGBT Wellbeing. It provided free HIV testing, ARVs, and the daily HIV-prevention pill (this is referred to as Pre-exposure Prophylaxis or PrEP). It’s one of several US-funded clinics that OUT operates around the country.
Its services are geared toward men who have sex with men. The reason is that rates of HIV are high among this group, and stigma may prevent some from seeking help in general healthcare settings.
When we visited the centre in Rosebank, a note was tied to the gate, stating: “Regrettably our clinic is temporarily closed and consequently no health services are available”. It encouraged patients to go to their nearest health facility.
According to OUT spokesperson Luiz De Barros, the clinics were forced to halt immediately after stop-work orders were issued. This prevented them from making alternative plans, leaving many people without ARVs or PrEP.
He said the centres had a total of 84 staff, who are now “at home without pay”, and about 5000 clients. Without their ARVs, De Barros worries that many clients are at risk of falling ill or developing drug-resistant HIV. Stopping HIV prevention services like PrEP will also “heighten the spread of HIV within communities,” he noted.
De Barros said they had not yet received any communication from USAID about the limited waiver, despite asking for information.
A clause in the waiver says it does not apply to “gender or DEI [diversity, equality and inclusion] ideology programs”. The Trump administration has not spelled out exactly what these terms mean, but it appears that DEI includes any health project which targets particular groups, like LGBTQ people.
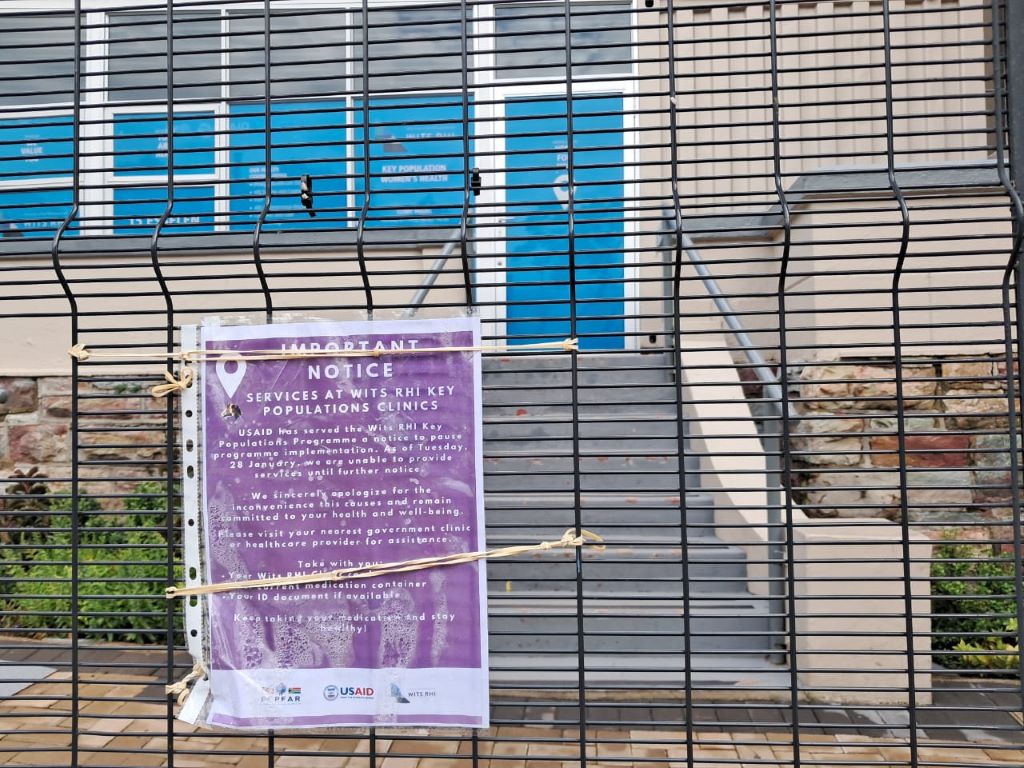
GroundUp and Spotlight visited a second health centre in Hillbrow run by the WITS Reproductive Health Institute (RHI). A sign on the gate stated: “USAID has served the WITS RHI Key Populations Programme a notice to pause programme implementation. As of Tuesday, 28 January, we are unable to provide services until further notice.”
WITS RHI’s annual reports suggest that USAID has previously sponsored its projects to treat and prevent HIV, including among high-risk groups like sex workers and transgender people.
The third health facility that we visited is the Ivan Toms Centre for Health, based in Green Point, Cape Town. A temporary closure notification hung from the door. The centre provided HIV and TB testing, ARVs, PrEP, and counselling services – all focused on men who have sex with men.
Representatives from a fourth organisation, NACOSA, told GroundUp and Spotlight that it had been forced to halt all of its USAID-funded services. Subsequently, USAID instructed the organisation to provide a revised budget which only includes activities listed under the waiver. As part of this limited budget, NACOSA proposed retaining a project which helps orphaned and vulnerable children living with HIV in the Western Cape.
Dr Ntlotleng Mabena, a technical specialist at NACOSA, said the project provides these children with psychological support and connects them to health providers. Clinical workers linked to the ANOVA health institute (which is also US-funded) provide the children with ARV treatment, she said.
NACOSA submitted the revised budget with the hope of restarting this service, but they are still awaiting approval. Mabena stated that ANOVA was also waiting for permission to continue. In the meantime, the service remains closed.
The US embassy in South Africa maintains that Trump’s funding cuts do not affect PEPFAR initiatives that provide life-saving services as defined in the limited waiver.
Yet all of the life-saving PEPFAR services that we investigated on Thursday are closed. The only services which have reopened are those funded by the CDC, which is unrelated to the waiver.
Published by GroundUp and Spotlight
Correction on 2025-02-21 12:29
Three paragraphs were removed from the article after publication because of confusion that arose as to whether they were on the record or not.
Republished from GroundUp under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Read the original article.