PVA Glue Boosts Effects of an Advanced Radiotherapy Treatment
Treatment for more advanced and difficult-to-treat head and neck cancers can be improved with the addition of polyvinyl alcohol (PVA), the same ingredient used in children’s glue. Researchers found that combining PVA with a boron-containing compound, D-BPA, improved the effects of a type of radiation therapy for cancer, compared to currently clinically used drugs. The PVA made the drug more selective of tumour cells and prolonged drug retention, helping to spare healthy cells from unnecessary radiation damage.
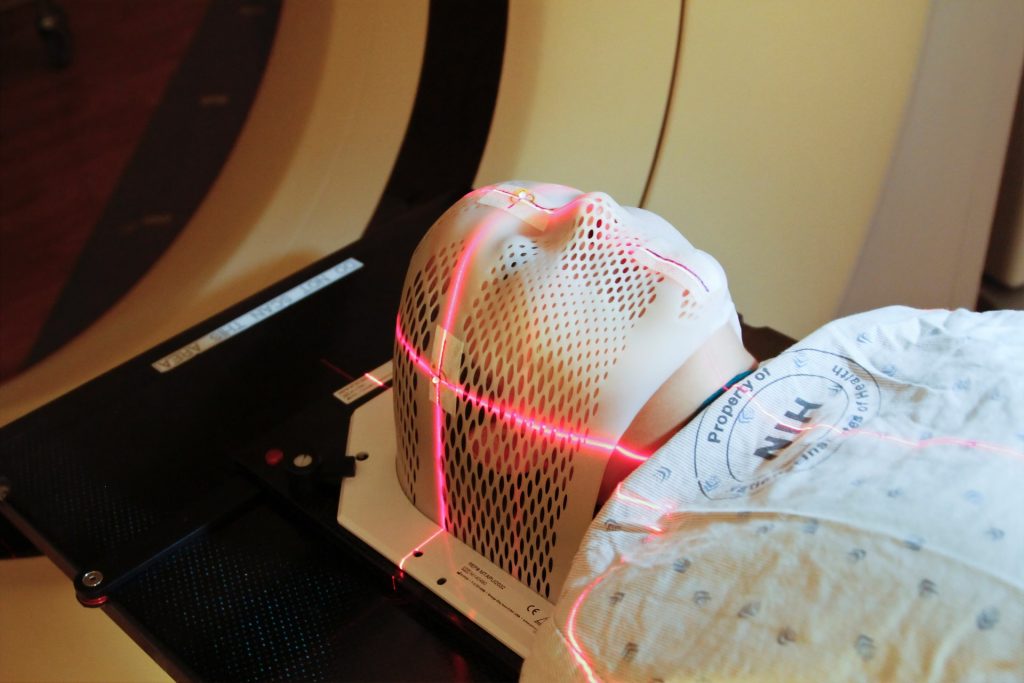
Japan became the first country to approve boron neutron capture therapy (BNCT), a type of targeted radiotherapy for cancer, in 2020. Doctors administer a boron-containing drug to patients, which is designed to selectively accumulate in tumour cells. The patients are then exposed to low-energy neutrons, which react with the boron, destroying cancer cells without damaging healthy cells.
The advantages of BNCT are that it targets only boron-containing cells, meaning that damage to healthy cells is less compared to some other treatments. It has also been found to be effective against some more challenging and recurring cancers. However, because low-energy neutrons are quite weak, their use is limited to certain areas of the body. Currently, they are approved for head and neck cancers, which are nearer the surface. Their effectiveness also depends on both the level and retention of boron within tumour cells for the duration of the treatment.
In newly published research, special research student Kakeru Konarita and Associate Professor Takahiro Nomoto from the University of Tokyo found that adding PVA to the boron-containing compound greatly improved both its accumulation and retention in cancer cells.
“We discovered that PVA, which is used in liquid glue, dramatically improves the efficacy of a compound called D-BPA, that until now has been removed from drug ingredients because it was considered useless,” explained Nomoto.
Neither PVA nor D-BPA exhibit pharmacological activity when administered alone. However, combining these compounds resulted in remarkably elevated tumour accumulation, prolonged retention and potent therapeutic efficacy, even when compared with a clinically used drug.”
Currently, the chemical substance L-BPA is the only approved boron compound for BNCT. It accumulates well within cancer cells, but, depending on the location of the cancer, can also enter some healthy cells. This makes it unsuitable for treating certain tumours. D-BPA is the enantiomer of L-BPA, meaning that its molecular structure is the mirror image of L-BPA but it is otherwise chemically identical. D-BPA appealed to the researchers because it appears to be more selective of cancer cells. However, on its own it doesn’t accumulate, which is why it was considered useless.
The team previously found that mixing PVA with L-BPA improved its effectiveness. In this latest research, they combined PVA with D-BPA and were surprised to see even higher levels of boron accumulating and more prolonged retention.
“There are many demands in the development of drugs for cancer treatment and much recent research and development has focused on complex combinations of expensive molecules,” said Nomoto. “However, we are concerned that such methods, when put into practice, will be so expensive that only a limited number of patients will benefit. In this study, we aimed to develop a drug with a simple structure and high functionality at a low cost.”
Now the team is promoting joint industry-academia collaboration to further this research and hope to apply this achievement to the treatment of other challenging cancers.
Source: University of Tokyo




