Surprisingly, Benefits of Dietary Fibre Vary Significantly between Individuals

Nutritionists generally advise everyone to eat more dietary fibre, but a new study suggests that its effects on health can vary, suggesting that recommendations should be tailored to each individual’s gut microbiome. The study, published in Gut Microbes, focused on resistant starch, a category of dietary fibre found in such foods as bread, cereals, green bananas, whole-grain pasta, brown rice and potatoes.
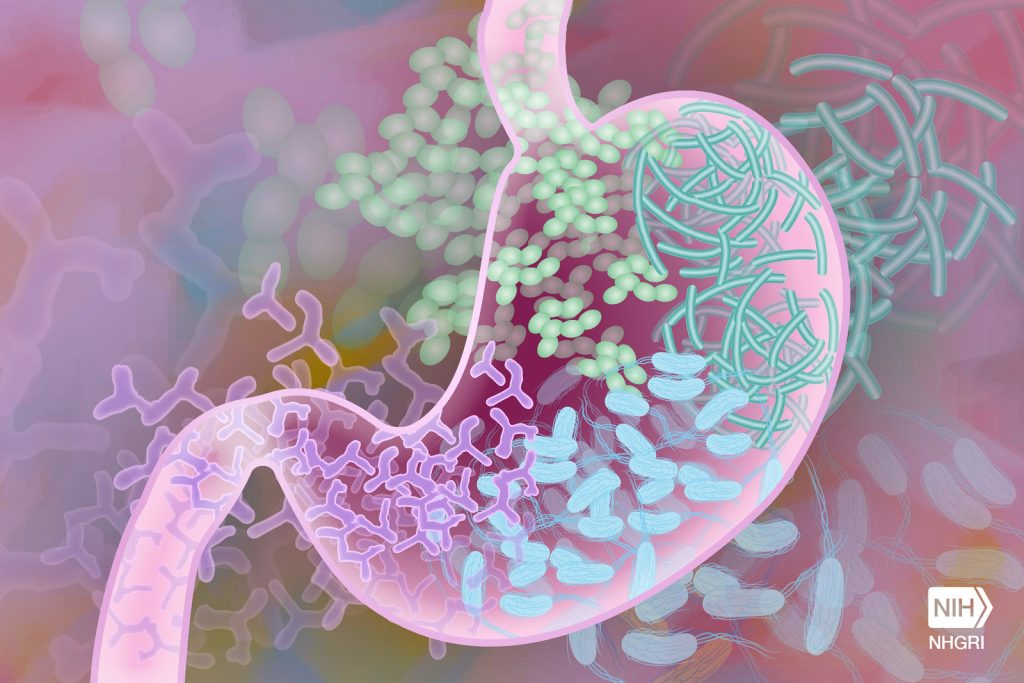
The researchers identified the gut microbe species that change in response to two different types of resistant starch. They found evidence that each individual may have a unique response to eating a resistant starch, with some people benefiting and others experiencing little or no effect. The reason for the variation appears tied to the level of diversity and composition of a person’s gut microbiome.
“Precision nutrition definitely has a use in determining what dietary fibre we should tell people to eat,” said Angela Poole, assistant professor of molecular nutrition and senior author of the study.
“This is critical because we’ve had public messaging advising people to eat more dietary fibre for decades,” Poole said. “At the same time, less than 10% of people eat the recommended intake. Since there are many different types of dietary fibre and carbohydrates, a better strategy would be to collect data on each person and tell them which dietary fibre they can eat to get the most bang for their buck.”
Resistant starch comes in five types, and resists degradation by human digestive enzymes until it reaches the gut. There, it acts as a substrate for certain gut microbes to produce short chain fatty acids, which are important in signaling pathways that regulate glucose and lipid metabolism. Multiple microbe species may work together to create the fatty acids.
In the study, Poole and colleagues tested three dietary treatments on 59 participants over seven weeks.
The team had three different types of crackers manufactured. Two crackers had the same ingredients, except one contained resistant starch type 2, which occurs naturally, and the other contained resistant starch type 4, which is human-made. A third control cracker was digestible by human enzymes, similar to white bread, and the researchers expected none of the bacteria to act on the control.
Subjects were then divided into two groups. The first group ate the resistant starch type 2 cracker first, followed by the control, and then resistant starch type 4. Each cracker type was eaten for 10 days, with five days of no cracker consumption between treatments. The second group reversed the order, also with the control in the middle.
They then sequenced the microbiomes of each participant before and after each treatment. For resistant starch type 2, more than 30 bacteria changed in abundance, including Ruminococcus bromii, which is considered a keystone resistant starch degrader in the human gut. For type 4, more than 20 bacteria changed. And for the control, nothing changed.
“For the resistant starch crackers, we could detect that 20 or 30 of them were changing, but how much they changed and whether they changed at all, for each of those bacteria, depended on the person,” Poole said.
Similarly, each resistant starch type changed different short chain fatty acids, with variable levels of fatty acid increases and decreases based on the individual. For resistant starch type 2, the researchers identified a subset of 13 bacteria that predicted change in amounts of propionate, a type of short chain fatty acid. Also for resistant starch 2, by knowing the diversity of an individual’s gut microbiome, the researchers could roughly predict if two types of short chain fatty acids (acetate and butyrate) were going to increase.
The most surprising result was that the control digestible cracker led to the greatest gains of short chain fatty acids. More work is needed to understand why, but Poole suspects that the order of cracker consumption was key to the result. Since many microbes are involved in making short chain fatty acids, she hypothesises that eating a resistant starch first primed the gut to produce the fatty acids when that person ate the digestible starch.
“That’s one of the major takeaways, maybe I can get away with eating a French baguette some of the time, and it may be better than just eating whole grain all the time,” Poole said. “But I have to test that, and it probably varies between people.”
Source: Cornell University