How Antibiotics in Infancy may Increase Diabetes Risk
Exposure to antibiotics during a key developmental window in infancy can stunt the growth of insulin-producing cells in the pancreas and may boost risk of diabetes later in life, new research in mice suggests. The study, published this month in the journal Science, also pinpoints specific microorganisms that may help those critical cells proliferate in early life.
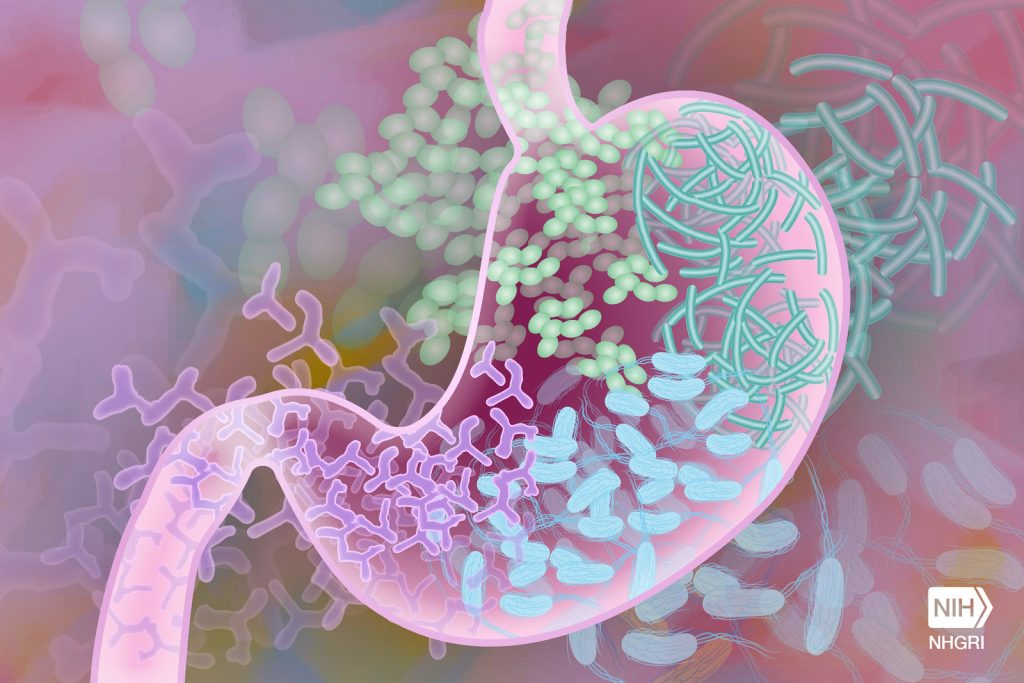
The findings are the latest to shine a light on the importance of the human infant microbiome—the constellation of bacteria and fungi living on and in us during our first few years. The research could lead to new approaches for addressing a host of metabolic diseases.
“We hope our study provides more awareness for how important the infant microbiome actually is for shaping development,” said first author Jennifer Hill, assistant professor in molecular, cellular and developmental biology at CU’s BioFrontiers Institute. “This work also provides important new evidence that microbe-based approaches could someday be used to not only prevent but also reverse diabetes.”
Something in the environment
More than 2 million U.S. adults live with Type 1 diabetes. The disease typically emerges in childhood, and genetics play a strong role. But scientists have found that, while identical twins share DNA that predisposes them to Type 1 diabetes, only one twin usually gets the disease.
“This tells you that there’s something about their environmental experiences that is changing their susceptibility,” said Hill.
For years, she has looked to microbes for answers.
Previous studies show that children who are breastfed or born vaginally, which can both promote a healthy infant microbiome, are less likely to develop Type 1 diabetes than others. Some research also shows that giving babies antibiotics early can inadvertently kill good bugs with bad and boost diabetes risk.
The lingering questions: What microbes are these infants missing out on?
“Our study identifies a critical window in early life when specific microbes are necessary to promote pancreatic cell development,” said Hill.
A key window of opportunity
She explained that human babies are born with a small amount of pancreatic “beta cells,” the only cells in the body that produce insulin. But some time in a baby’s first year, a once-in-a-lifetime surge in beta cell growth occurs.
“If, for whatever reason, we don’t undergo this event of expansion and proliferation, that can be a cause of diabetes,” Hill said.
She conducted the current study as a postdoctoral researcher at the University of Utah with senior author June Round, a professor of pathology.
They found that when they gave broad-spectrum antibiotics to mice during a specific window (the human equivalent of about 7 to 12 months of life), the mice developed fewer insulin producing cells, higher blood sugar levels, lower insulin levels and generally worse metabolic function in adulthood.
“This, to me, was shocking and a bit scary,” said Round. “It showed how important the microbiota is during this very short early period of development.”
Lessons in baby poop
In other experiments, the scientists gave specific microbes to mice, and found that several they increased their production of beta cells and boosted insulin levels in the blood. The most powerful was a fungus called Candida dubliniensis.
The team used faecal samples from The Environmental Determinants of Diabetes in the Young (TEDDY) study to make what Hill calls “poop slushies” and fed them to the mice.
When the researchers inoculated newborn mice with poop from healthy infants between 7 to 12 months in age, their beta cells began to grow. Poop from infants of other ages did not do the same. Notably, Candida dublineinsis was abundant in human babies only during this time period.
“This suggests that humans also have a narrow window of colonisation by these beta cell promoting microbes,” said Hill.
When male mice that were genetically predisposed to Type 1 diabetes were colonised with the fungus in infancy, they developed diabetes less than 15% of the time. Males that didn’t receive the fungus got diabetes 90% of the time.
Even more promising, when researchers gave the fungus to adult mice whose insulin-producing cells had been killed off, those cells regenerated.
Too early for treatments
Hill stresses that she is not “anti-antibiotics.” But she does imagine a day when doctors could give microbe-based drugs or supplements alongside antibiotics to replace the metabolism-supporting bugs they inadvertently kill.
Poop slushies (faecal microbiota transplants) have already been used experimentally to try to improve metabolic profiles of people with Type 2 diabetes, which can also damage pancreatic beta cells.
But such approaches can come with real risk, since many microbes that are beneficial in childhood can cause harm in adults. Instead, she hopes that scientists can someday harness the specific mechanisms the microbes use to develop novel treatments for healing a damaged pancreas—reversing diabetes.
She recently helped establish a state-of-the-art “germ-free” facility for studying the infant microbiome at CU Boulder. There, animals can be bred and raised entirely without microbes, and by re-introducing them one by one scientists can learn they work.
“Historically we have interpreted germs as something we want to avoid, but we probably have way more beneficial microbes than pathogens,” she said. “By harnessing their power, we can do a lot to benefit human health.”