A New Understanding of Graft-versus-host Disease
New research published in the journal Immunity challenges the prevailing hypothesis for how donor stem cell grafts cause graft-versus-host disease (GVHD) and offers an alternative model that could guide development of novel therapies.
The study showed in a mouse model that GVHD, which often affects the skin, gut and liver, is maintained by donor T cells that seed those tissues soon after transplant and not by the continual recruitment of T cells from the blood as previously thought.
“This study changes the paradigm of how people think about GVHD,” said co-senior author Warren Shlomchik, MD, professor of medicine and immunology at the University of Pittsburgh School of Medicine. “It provides important mechanistic detail about what’s going on in the tissues affected by GVHD, which could ultimately inform the development of better therapeutics and lead to better outcomes for stem cell recipients.”
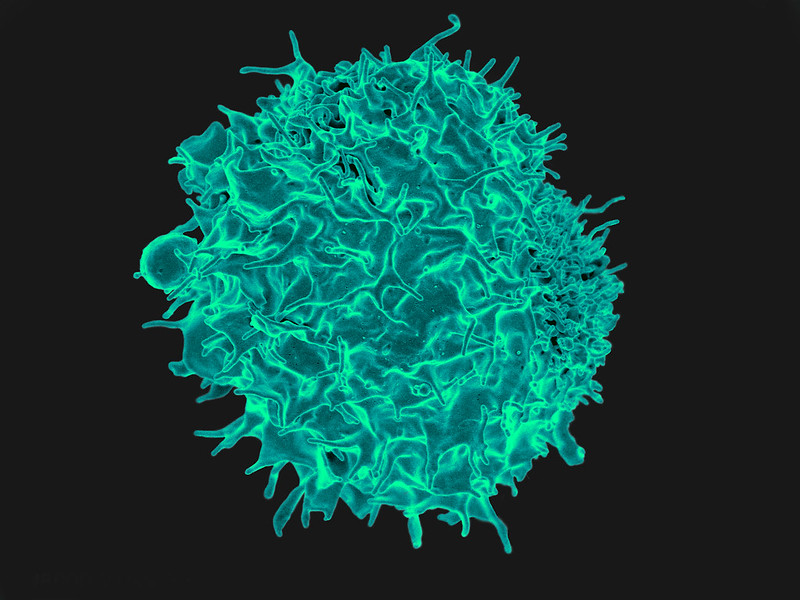
Allogeneic stem cell transplantation involves infusion of stem cells from a healthy donor’s blood or bone marrow to a recipient. While often lifesaving for patients with leukaemia and other blood disorders, the treatment also comes with a risk of developing GVHD, a life-threatening disease that occurs when donor alloreactive T cells attack the recipient’s healthy tissues.
According to a widely held theory, GVHD is maintained by T cells that continually migrate from secondary lymphoid organs throughout the body, including the spleen and lymph nodes, to affected tissues via the blood.
However, a different model posits that the disease is maintained locally by T cells in the tissues with little input from the blood. In the new study, Shlomchik, lead author Faruk Sacirbegovic, PhD, research assistant professor of surgery at Pitt, and their team investigated the two hypotheses for how GVHD is sustained in tissues.
The researchers developed a system to track alloreactive T cells in a mouse model of GVHD by labelling individual cells with unique tags to create different T cell “flavours.” By measuring the tags over time, they monitored where the T cells travelled and replicated.
The analysis showed that each tissue affected by GVHD had unique T cell populations with varying frequencies of each T cell flavour.
“This finding is strong evidence that the disease is locally maintained by T cells in each of the tissues,” explained Shlomchik. “If tissues were constantly getting T cells from circulating blood, then the frequencies of T cell flavors in each tissue should become more and more alike over time — but we didn’t see that.”
The team used mathematical models to predict that progenitor T cells seed out into recipient tissues early after transplant, differentiating there into disease-causing cells.
Next a series of experiments was conducted to confirm this prediction and identified these progenitors as T cells expressing a gene called Tcf7.
“We think that progenitor T cells are long-lived in target tissues and are critical for maintaining GVHD,” said co-senior author Thomas Höfer, PhD, professor of theoretical systems biology at the University of Heidelberg. “After the initial seeding phase, the disease is mostly sustained within the tissue itself without a lot of input from new T cells in the blood.”
Stem cell recipients are typically treated with immunosuppressants to prevent and treat GVHD. As these powerful drugs act systemically to suppress the immune system, they also lower immunity to infections and have other side effects.
According to the researchers, the study’s insights could eventually lead to new, targeted therapies for GVHD.
“Now that we know the identity of progenitor cells, we might be able to prevent them forming early post-transplant or target them directly after they’ve formed,” said Shlomchik. “The findings also suggest that treating GVHD in the tissues themselves would be effective – although targeting tissues beyond the skin remains a challenge.”
With better ways to minimise the risk of GVHD after stem cell transplantation, the procedure could become more widely used to treat a broader range of diseases, including blood disorders such as sickle cell anaemia and autoimmune diseases such as lupus and multiple sclerosis.
Source: University of Pittsburgh

