Scars of Destroyed Brain Tumours are Fertile Grounds for Recurrence

A Ludwig Cancer Research study has discovered that recurrent tumours of the aggressive brain cancer glioblastoma multiforme (GBM) grow out of the fibrous scars of malignant predecessors destroyed by interventions such as radiotherapy, surgery and immunotherapy.
Led by Ludwig Lausanne’s Johanna Joyce, Spencer Watson and alumnus Anoek Zomer and published in the current issue of Cancer Cell, the study describes how these scars enable the regrowth of tumours and identifies drug targets to sabotage their malignant support. It also demonstrates the efficacy of such combination therapies in preclinical trials using mouse models of GBM.
“We’ve identified fibrotic scarring as a key source of GBM resurgence following therapy, showing how it creates a protective niche for the regrowth of the tumor,” said Joyce. “Our findings suggest that blocking the process of scarring in the brain by adding anti-fibrosis agents to current treatment strategies could help prevent glioblastoma from recurring and improve the outcomes of therapy.”
There is a great need for such interventions. GBM is the most common and aggressive form of brain cancer in adults. Despite considerable effort to develop effective therapies for the cancer, the average life expectancy of patients remains around 14 months following diagnosis.
The origins of the current study date back to 2016, when the Joyce lab reported in the journal Science its examination in mouse models of strategies to overcome resistance to a promising immunotherapy for the treatment of GBM. That experimental therapy, which inhibits signalling by the colony stimulating factor-1 receptor (CSF-1R) and currently in clinical trials, targets immune cells known as macrophages and their brain-resident versions, microglia, both of which are manipulated by GBM cells to support tumour growth and survival.
The Joyce lab has demonstrated that CSF-1R inhibition reprograms these immune cells into an anti-tumour state and so induces significant tumour regression. Yet, as the Science study showed, about half the mice show relapse following an initial response to the therapy. “What was most remarkable about that observation was that every single time a brain tumour recurred following immunotherapy, it regrew right next to a scar that had formed at the original site of a tumour,” said Joyce.
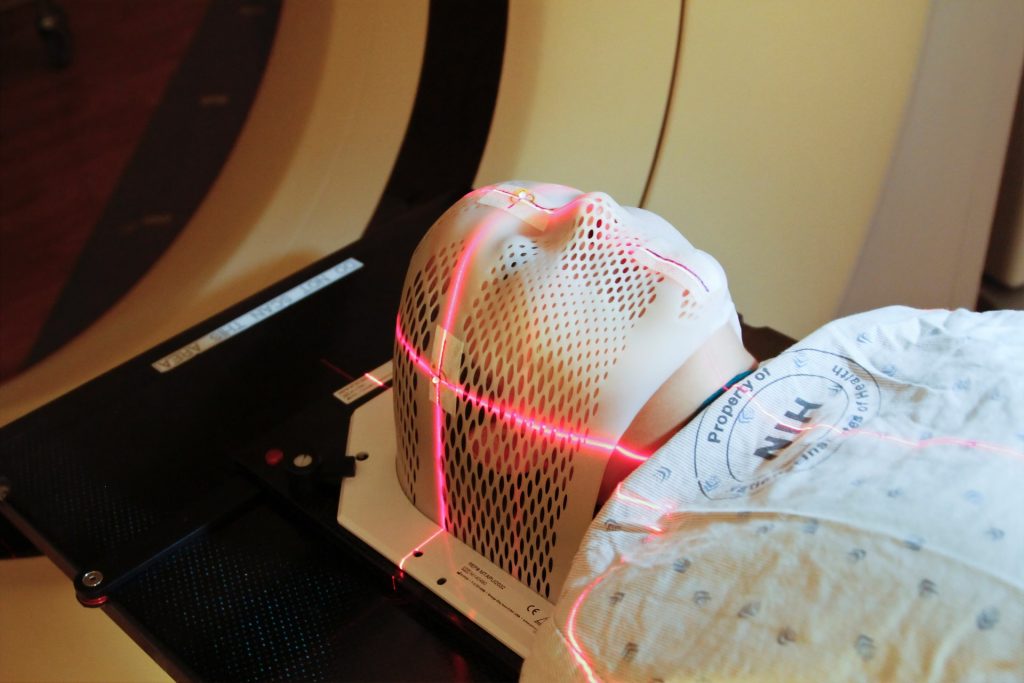
In the current study, Joyce, Watson, Zomer and their colleagues examined tumour samples obtained from patients undergoing GBM therapy and showed that fibrotic scarring occurs following therapy in humans as well – and that it is similarly associated with tumour recurrence. They also showed that the fibrotic scarring occurs in response to not only immunotherapy but also following the surgical and radiological removal of tumours.
To explore how fibrosis contributes to relapse, the researchers applied an integrated suite of advanced technologies to analyze the cellular and molecular geography of the scars and the microenvironment of resurgent tumors.
These technologies include the analysis of global gene expression in individual cells, the comprehensive analysis of proteins in the tissues as well a workflow and AI-powered suite of analytical methods for the spatial analysis of tissues named hyperplexed immunofluorescence imaging (HIFI). Recently developed by Watson and colleagues in the Joyce lab, HIFI permits the simultaneous visualisation of multiple molecular markers in and around cells across broad cross-sections of tissues, enabling the generation of granular maps of the tumour microenvironment.
“Applied together, these advanced methods allowed us to see exactly how fibrotic scars form,” said Watson. “They revealed that the fibrosis serves as a kind of protective cocoon for residual cancer cells and pushes them into a dormant state in which they are largely resistant to therapy. We found that it also shields them from surveillance and elimination by the immune system.”
Integrated analyses of the tissue microenvironment following therapy revealed that the descendants of cells associated with tumor-feeding blood vessels become functionally altered to resemble fibroblasts—fiber-producing cells commonly involved in wound-healing. These perivascular-derived fibroblast-like (PDFL) cells fan out across the region previously occupied by the regressing tumor, where they mediate the generation of fibrotic scars. These cells, the researchers found, are especially activated by neuroinflammation and immune factors known as cytokines, most notably one called transforming growth factor-β (TGF-β).
“To see if targeting fibrotic scarring could improve therapeutic outcomes for GBM, we devised a treatment regimen using existing drugs to block TGF-β signaling and suppress neuroinflammation in combination with CSF-1R inhibition and evaluated it in preclinical trials using mouse models of GBM,” said Joyce. “We also timed these additional treatments to coincide with the period of maximal PDFL activation identified by our studies. Our results show that the drug combination inhibited fibrotic scarring, diminished the numbers of surviving tumor cells and extended the survival of treated mice compared to controls.”
The researchers suggest that approaches to limit fibrotic scarring could significantly improve outcomes for GBM patients receiving surgical, radiation or macrophage-targeting therapies. Additional research, they note, will likely yield even better drug targets for such combination therapies.