Familial High Cholesterol Often Eludes Genetic Testing
Most familial hypercholesterolemia (FH) cases would go undetected if people were to rely on array-based genetic tests alone, a new study suggests.
FH predisposes people to elevated levels of LDL cholesterol, which can lead to premature coronary artery disease and early death.
For example, the 23andMe test, which has a limited screen for only 24 known FH variants, would have missed over 60% of individuals with the autosomal dominant disorder. This figure was even worse for non-European ancestry individuals.
“Limited-variant screens may falsely reassure the majority of individuals at risk for FH that they do not carry a disease-causing variant, especially individuals of self-reported Black/African American and Hispanic ancestry,” according to Amy Sturm, of the Geisinger Genomic Medicine Institute in Danville, Pennsylvania, and colleagues.
In their study, limited-variant screening would miss nearly 94% and 85% of Black and Hispanic individuals with confirmed FH pathogenic variants. However this would be true for only a third of Ashkenazi Jewish people.
“The reduced yield of limited-variant screening could result in a major health care disparity for groups already affected by social and medical disenfranchisement that beget serious health disparities including a significantly higher rate of cardiovascular death among Black/African American individuals,” the investigators said.
“When FH is strongly clinical suspected, even if array-based FH reporting has negative results, a clinical genetic test should still be considered,” according to an accompanying note by JAMA Cardiology editors Pradeep Natarajan, MD, MMSc, of Massachusetts General Hospital and Harvard Medical School in Boston, and Elizabeth McNally, MD, PhD, of Northwestern University Feinberg School of Medicine in Chicago.
“Genetic databases overrepresent European ancestry populations and therefore make interpretation of genetic variation more accurate in these cohorts. However, even 64% of the FH mutations in European American individuals would have been missed by the 24-variant [test],” noted Drs Natarajan and McNally.
“Unfortunately, genetic testing for FH is underused, with 90% of affected individuals worldwide remaining undiagnosed and only 3.9% of patients with FH in the U.S. having a record of genetic testing,” noted Dr Sturm and colleagues.
“Recent expert statements recommend that patients suspected of having FH be offered genetic testing and that first-degree relatives of genetically positive individuals be screened for FH by lipid profile or genetic testing,” according to them.
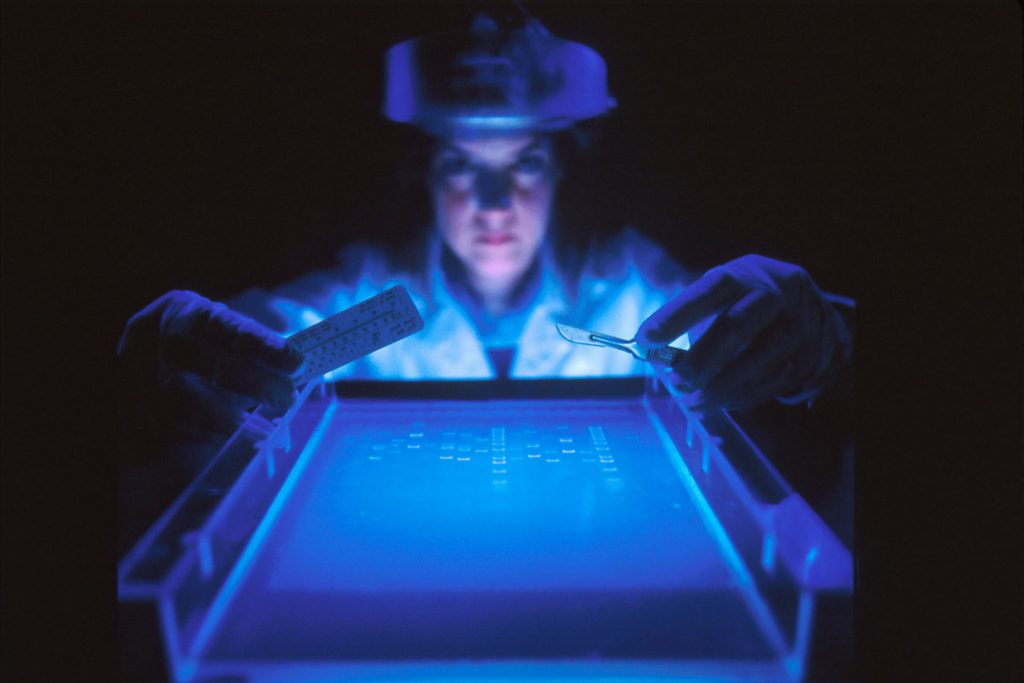
Comprehensive genetic testing with next-generation sequencing (NGS) detects over 2000 potentially pathogenic variants within full genomes. Assay-based screens such as 23andMe only test for a small subset of known variants, and not the number present.
Both types of genetic tests for FH are available either in clinical settings or as a direct service to consumers.
“Whether testing is obtained directly by a consumer or through a clinical setting, those tested should consult with a genetic counselor or other qualified health care professional to fully understand the benefits and limitations of the different types of genetic testing for FH,” Sturm’s group urged.
For the study, the authors took deidentified NGS results, sourced from a single clinical laboratory, for gene panels of individuals receiving comprehensive genetic testing either for an FH indication (4563 participants) or as proactive health screening (6482 participants).
The researchers had tested both cohorts for more than 2000 possible variants in four FH-associated genes: LDLR, APOB, PCSK9, and LDLRAP1.
With the limited screening tests, only 8.4% of people with FH indication had a positive detection, compared to 27.0% for comprehensive NGS genotyping. In the proactive cohort of people with no clinical suspicion of FH, clinically significant FH variant prevalence was about one in 191 according to the comprehensive test.
A limitation was the researchers’ inability to confirm genetic testing results with medical and family histories.
Source: MedPage Today
Journal information: Sturm AC, et al “Limited-variant screening vs comprehensive genetic testing for familial hypercholesterolemia diagnosis” JAMA Cardiol 2021; DOI: 10.1001/jamacardio.2021.1301.

