A Short Course of Radiation Therapy for Endometrial Cancer Patients is Effective
In a randomised clinical trial, researchers from Huntsman Cancer Institute at the University of Utah (the U) have found that short-course, higher dose vaginal brachytherapy for endometrial cancer had similar effectiveness to more frequent, lower dose sessions.
Gita Suneja, MD, MS, physician-scientist at Huntsman Cancer Institute and professor of radiation oncology at the U, is the first author of the SAVE trial report – which stands for, Short-Course Adjuvant Vaginal Cuff Brachytherapy in Early Endometrial Cancer Compared with Standard of Care.
“There isn’t high quality-data on optimal dose and schedule for brachytherapy treatments. Because of this, practice patterns really vary,” says Suneja. “The SAVE trial sought to try to lower the number of treatments that patients were receiving but maintain short-term quality of life and disease control.”
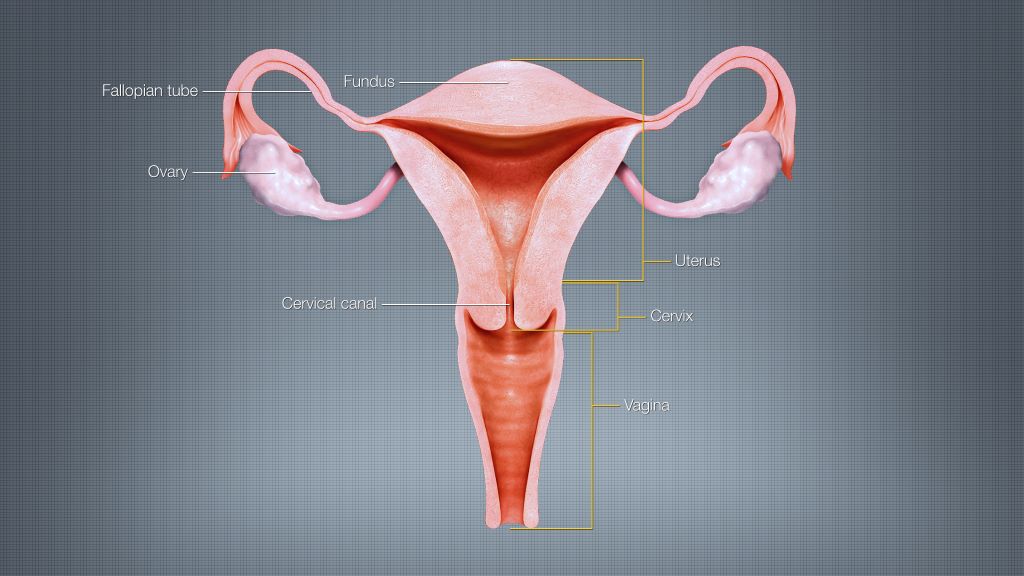
Endometrial cancer is a disease that begins in the lining of the uterus. The primary treatment for endometrial cancer is surgery, including the removal of the uterus, cervix, and upper vagina. Brachytherapy, a form of internal radiation, is used as a secondary treatment to prevent the cancer’s return. Patients receiving vaginal cuff brachytherapy are treated with internal radiation by way of an applicator in the vaginal cavity.
The SAVE trial compared two groups who received different treatment doses over a varying number of sessions. The control group received the standard treatment – between three to five appointments with lower doses. The experimental group received higher doses of radiation in just two sessions.
“The study outcomes will help improve cancer care for Huntsman Cancer Institute patients across the five states of the Mountain West.”
Gita Suneja, MD, MS
The researchers found similarly effective short-term outcomes and few acute toxicities for the patients in the experimental group.
David Gaffney, MD, PhD, FACR, FABS, FASTRO, physician-scientist at Huntsman Cancer Institute and professor of radiation oncology at the U, developed the idea for the SAVE study after seeing patient need. According to the American Cancer Society, endometrial cancer is the most common cancer of the female reproductive organs. Incidence is on the rise, as is the mortality rate.
“It is a big win when we can preserve good outcomes and make cancer care easier,” says Gaffney.
The results of the SAVE trial were published in JCO Oncology Advances.
Source: Huntsman Cancer Institute




