Antibiotic Resistance Among Key Bacterial Species Plateaus Over Time
Use of antibiotics was weakly associated with resistance, indicating additional factors may be at play

Antibiotic resistance tends to stabilise over time, according to a study published April 3, 2025 in the open-access journal PLOS Pathogens by Sonja Lehtinen from the University of Lausanne, Switzerland, and colleagues.
Antibiotic resistance is a major public health concern, contributing to an estimated 5 million deaths per year. Understanding long-term resistance patterns could help public health researchers to monitor and characterise drug resistance as well as inform the impact of interventions on resistance.
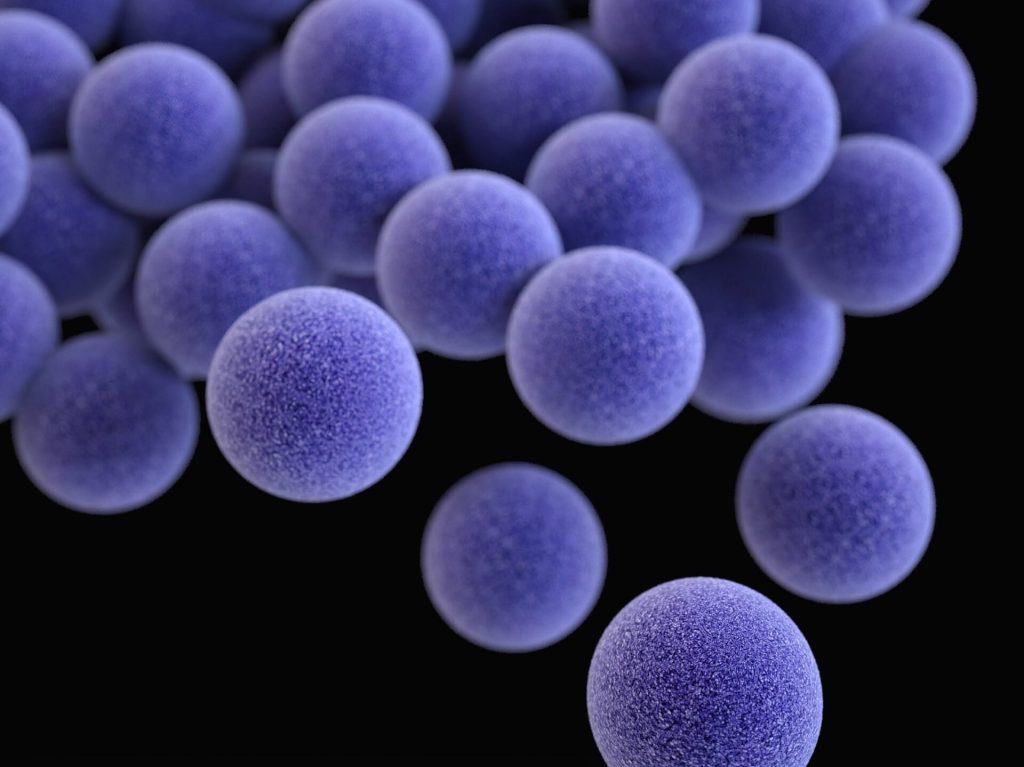
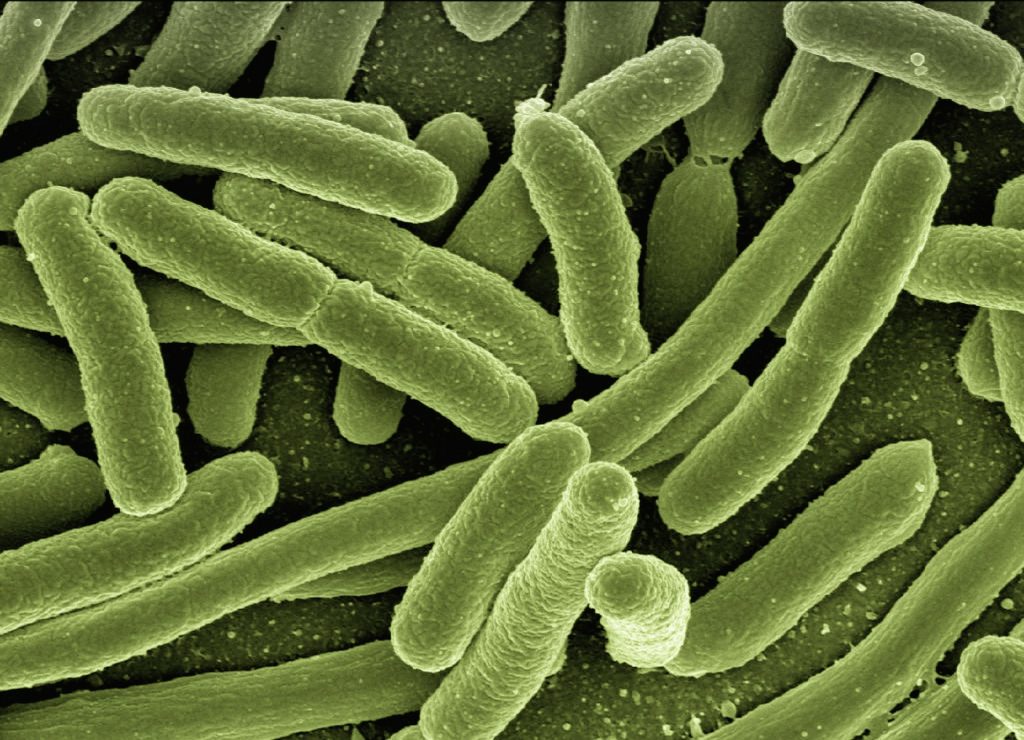
In this study, researchers analysed drug resistance in more than 3 million bacterial samples collected across 30 countries in Europe from 1998 to 2019. Samples encompassed eight bacteria species important to public health, including Streptococcus pneumoniae, Staphylococcus aureus, Escherichia coli, and Klebsiella pneumoniae.
They found that while antibiotic resistance initially rises in response to antibiotic use, it does not rise indefinitely. Instead, resistance rates reached an equilibrium over the 20-year period in most species. Antibiotic use contributed to how quickly resistance levels stabilised as well as variability in resistance rates across different countries. But the association between changes in drug resistance and antibiotic use was weak, suggesting that additional, yet unknown, factors are at play.
The study highlights that continued increase in antibiotic resistance is not inevitable and provides new insights to help researchers monitor drug resistance.
Senior author Francois Blanquart notes: “When we looked into the dynamics of antibiotic resistance in many important bacterial pathogens all over Europe and in the last few decades, we often found that resistance frequency initially increases and then stabilises to an intermediate level. The consumption of the antibiotic in the country explained both the speed of initial increase and the level of stabilisation.”
Senior author Sonja Lehtinen summarises: “In this study, we were interested in whether antibiotic resistance frequencies in Europe were systematically increasing over the long-term. Instead, we find a pattern where, after an initial increase, resistance frequencies tend to reach a stable plateau.”
Provided by PLOS