Magnetic Fields Boost Doxorubicin Uptake in Breast Cancer Treatment
Researchers at the National University of Singapore (NUS) have developed a non-invasive method to improve the effectiveness of chemotherapy while reducing its harmful side effects.
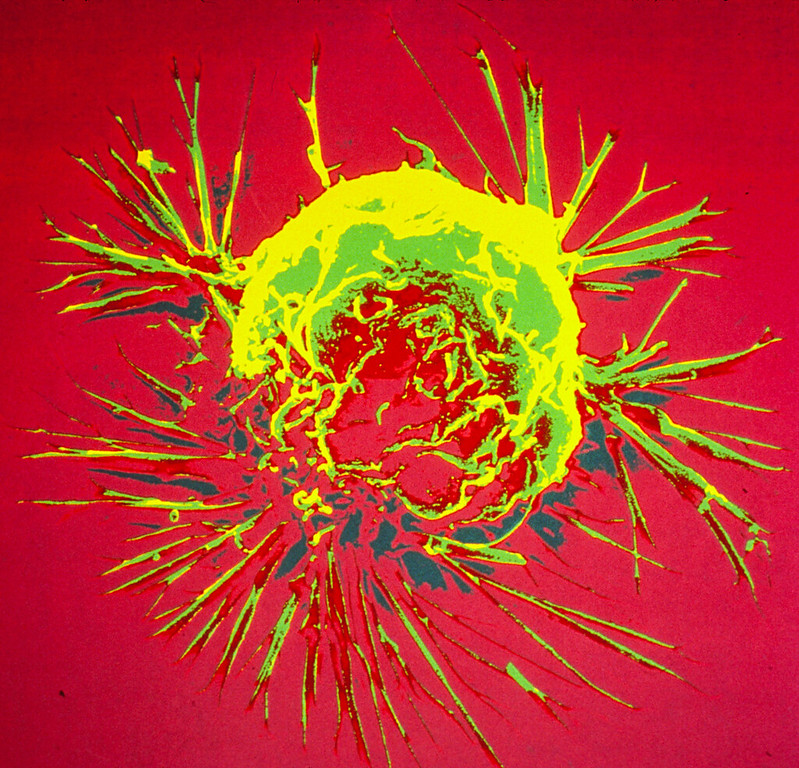
By applying brief, localised pulses of magnetic fields, the team demonstrated a significant increase in the uptake of doxorubicin (DOX), a widely used chemotherapy drug, into breast cancer cells, with minimal impact on healthy tissues. This selective uptake enables more precise targeting of cancer cells, potentially improving treatment outcomes and reducing the adverse effects often associated with chemotherapy.
The study, led by Associate Professor Alfredo Franco-Obregón at NUS, is the first to systematically show how pulsed magnetic fields enhance DOX uptake in cancer cells. The team also showed that this approach could suppress tumours at lower drug doses.
The team’s research was published in the journal Cancers. It builds on earlier work from 2022, which first revealed that certain cancer cells are more vulnerable to magnetic field therapy.
Better chemotherapy outcomes and fewer side effects
DOX is a commonly used chemotherapy drug for breast cancer. It works by binding to DNA components and disrupting cell replication and respiration, which then kills off cancer cells. Despite its efficacy, it is a non-selective drug, which means it can also damage healthy tissues, leading to side effects ranging from mild to severe, including cardiomyopathy and muscle atrophy.
To address these challenges, the NUS researchers developed a novel approach that uses brief pulses of magnetic fields to selectively increase DOX uptake into breast cancer cells. Their study revealed the role of a calcium ion channel known as TRPC1, which is often found in aggressive cancers, including breast cancer. Magnetic field exposure activates TRPC1, enhancing its ability to facilitate the entry of DOX into cancer cells.
The researchers conducted experiments comparing the effects of the magnetic field therapy on human breast cancer cells and healthy muscle cells. They found that breast cancer cells took in significantly more DOX when exposed to magnetic pulses, while normal tissues were not targeted as much. A 10-minute magnetic field exposure reduced the drug concentration needed for similar amount of cancer killing by half, particularly at low doses of the drug.
In contrast, healthy muscle cells did not show an increase in cell death in response to the combination of DOX and magnetic pulses indicating greater protection for non-cancerous tissues.
The team also demonstrated that reducing TRPC1 expression or blocking its activity eliminated this effect, which confirms the crucial role of TRPC1 channels in the process. “Importantly, when we increased the amount of TRPC1, we observed an increase in DOX uptake – this means that TRPC1 can be used as a viable therapeutic target for aggressive cancers,” said first author Mr Viresh Krishnan Sukumar, PhD candidate at NUS Centre for Cancer Research (N2CR).
“What’s promising is that this mechanism works strongest at low drug concentrations, enabling us to target cancer cells more effectively while reducing the burden of chemotherapy on healthy tissues,” Assoc Prof Franco-Obregón added.
With breast cancer remaining the leading cause of cancer-related deaths among women worldwide, the need for novel treatment strategies is urgent. “The majority of women who undergo chemotherapy experience side effects from treatment, and in some cases, doses of chemotherapy need to be reduced, or in severe cases, stopped prematurely,” said Assistant Professor Joline Lim, Principal Investigator at N2CR and Senior Consultant, Department of Haematology-Oncology, National University Cancer Institute, Singapore. “Moreover, prolonged exposure to high-dose chemotherapy can also lead to drug resistance. This targeted approach represents an excellent opportunity to potentially improve treatment outcomes while preserving patients’ quality of life.”
Advancing the frontier of precision oncology
The team’s magnetic-assisted approach addresses one of the biggest challenges of chemotherapy, namely its toxic effects on healthy tissues. By selectively enhancing drug uptake into cancer cells, this method has the potential to drastically reduce the systemic side effects often experienced by breast cancer patients. This not only improves treatment outcomes and quality of life, but also encourages earlier treatment for those hesitant about treatment side effects. The study also underscores the role of biomarkers, such as elevated TRPC1 expression, in transforming cancer care by enabling precision-driven treatment options.
Future work will focus on translating these findings into clinical practice by localising magnetic field exposure specifically to tumours in patients. This would further validate the potential to reduce systemic DOX doses while maximising localised drug delivery in cancer cells.
“Our approach will be patented and form the foundation for a startup specialising in breast cancer treatment. We are currently in discussions with potential investors in Southeast Asia and the United States to translate this technology from bench to bedside,” shared Assoc Prof Franco-Obregón. National University Cancer Institute, Singapore. “Moreover, prolonged exposure to high-dose chemotherapy can also lead to drug resistance. This targeted approach represents an excellent opportunity to potentially improve treatment outcomes while preserving patients’ quality of life.”
Source: National University of Singapore


