High Burden of Uncontrolled Disease in KwaZulu-Natal

A comprehensive health-screening program has found a high burden of poorly controlled or uncontrolled disease KwaZulu-Natal, along with a high incidence of undiagnosed diseases.
The study, published in The Lancet Global Health, found that four out of five women over 30 had a chronic health condition, and that the HIV-negative population and older people had the highest burden of undiagnosed or poorly controlled non-communicable diseases such as diabetes and hypertension. The study was conducted at the Africa Health Research Institute (AHRI).
Study co-leader Emily Wong, MD, at AHRI in Durban, said: “The data will give AHRI researchers and the Department of Health critical indicators for where the most urgent interventions are needed,” Dr Wong said. “The research was done before COVID, but it has highlighted the urgency of diagnosing and treating people with non-communicable diseases — given that people with uncontrolled diabetes and hypertension are at higher risk of getting very ill with COVID.”
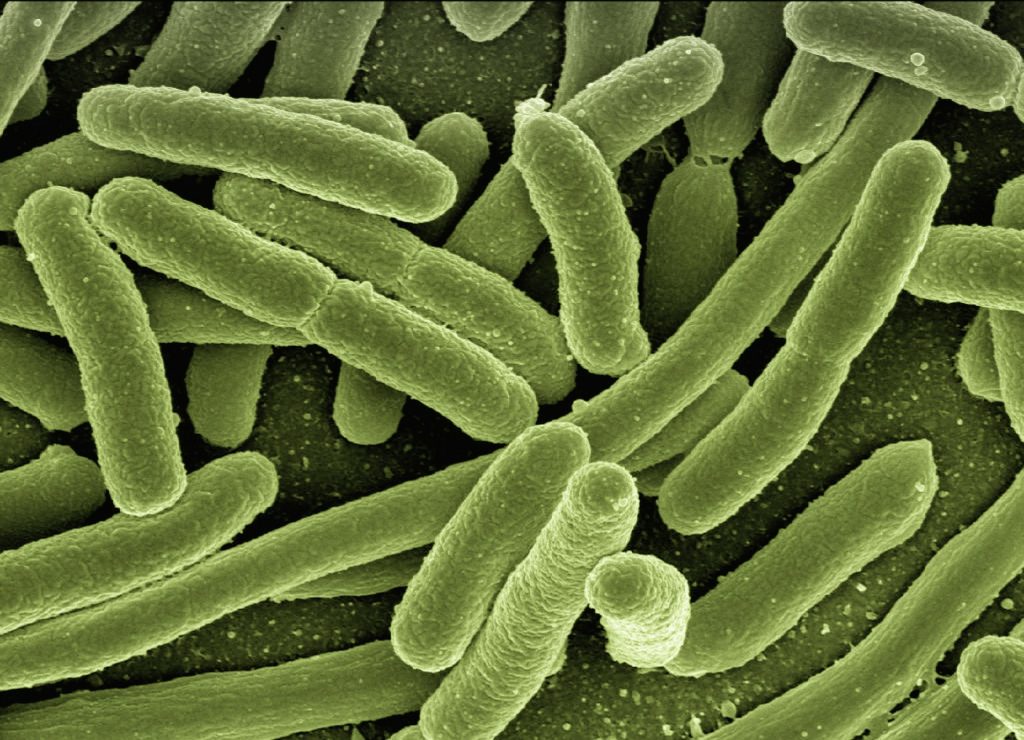
HIV-associated tuberculosis infections are particularly prevalent in Durban. Dr Wong of the University of Alabama works there to understand the impact of HIV infection on tuberculosis pathogenesis, immunity and epidemiology. In sub-Saharan Africa, 15 years of intense public health efforts that increased access to antiretroviral therapy has resulted in decreased AIDS mortality and raised life expectancy. As a result, there is an increasing priority to address other causes of disease, including tuberculosis and non-communicable diseases.
Over 18 months, health workers screened 17 118 people aged 15 years and older via mobile camps within 1 kilometre of each participant’s home in the uMkhanyakude district. They found high and overlapping burdens of HIV, tuberculosis, diabetes and hypertension among men and women.
While the HIV cases were largely well diagnosed and treated, some demographic groups still had high rates of undiagnosed and untreated HIV, such as men in their 20s and 30s. In contrast, the majority of people with tuberculosis, diabetes or hypertension were either undiagnosed or not well controlled. Of particular concern was the high rates of undiagnosed and asymptomatic tuberculosis discovered, as it remains one of the leading causes of death in South Africa.
“Our findings suggest that the massive efforts of the past 15 years to test and treat for HIV have done very well for that one disease,” Dr Wong said. “But in that process, we may have neglected some of the other important diseases that are highly prevalent.”
The mobile camps screened for diabetes, high blood pressure, nutritional status (obesity and malnutrition), and tobacco and alcohol use, as well as HIV and tuberculosis. The tuberculosis screening component included high-quality digital chest X-rays and sputum tests for people who reported symptoms or had abnormal X-rays. Clinical information was combined with 20 years of population data from AHRI’s health and demographic surveillance research. Using a sophisticated data system combined with artificial intelligence to interpret the chest X-rays, AHRI’s clinical team examined the information in real time, referring people to the public health system as needed.
The study found that:
- Half of the participants had at least one active disease, and 12 percent had two or more diseases. Diabetes and hypertension incidences were 8.5 percent and 23 percent, respectively.
- One-third of the people were living with HIV, but this was mostly well diagnosed and treated. A particularly high burden of HIV, high blood pressure and diabetes was seen in women.
- For tuberculosis, 1.4 percent of the people had active disease, and 22 percent had lifetime disease. About 80 percent of the undiagnosed tuberculosis was asymptomatic, with higher rates of active tuberculosis seen in men.
- Several disease patterns varied by geographical location — eg, the highest HIV burden was seen near main roads, while higher rates of tuberculosis and non-communicable diseases were seen in more remote areas.
Source: University of Alabama at Birmingham
Journal information: Wong, E. B., et al. (2021) Convergence of infectious and non-communicable disease epidemics in rural South Africa: a cross-sectional, population-based multimorbidity study. The Lancet Global Health. doi.org/10.1016/S2214-109X(21)00176-5.