Tiny Magnetic Discs Offer Remote Brain Stimulation without Genetic Modifications

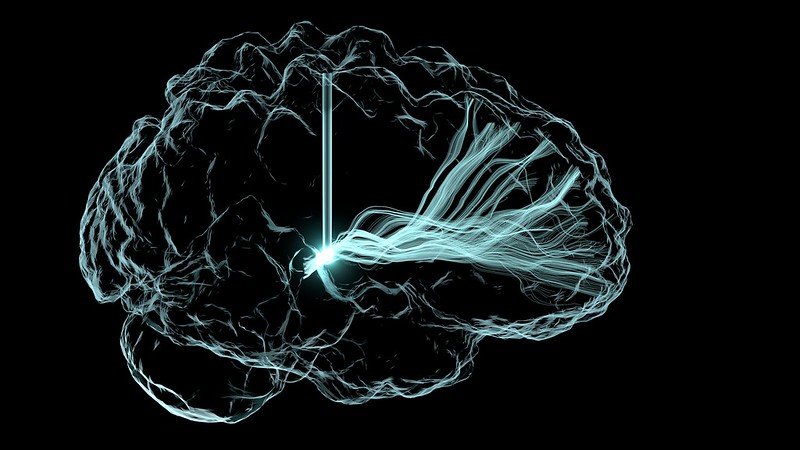
Novel magnetic nanodiscs could provide a much less invasive way of stimulating parts of the brain, paving the way for stimulation therapies without implants or genetic modification, MIT researchers report in Nature Nanotechnology.
The scientists envision that the tiny discs – about 250nm across – would be injected directly into the chosen brain location. From there, they could be activated at any time simply by applying an external magnetic field. The new particles could quickly find applications in biomedical research, and eventually, after sufficient testing, might be applied to clinical uses.
The research is described in the paper by Polina Anikeeva, a professor in MIT’s departments of Materials Science and Engineering and Brain and Cognitive Sciences, graduate student Ye Ji Kim, and 17 others at MIT and in Germany.
Deep brain stimulation (DBS) uses electrodes implanted in the target brain regions to treat symptoms of neurological and psychiatric conditions such as Parkinson’s disease and obsessive-compulsive disorder. Despite its efficacy, the surgical difficulty and clinical complications associated with DBS limit the number of cases where such an invasive procedure is warranted. The new nanodiscs could provide a much more benign way of achieving the same results.
Over the past decade other implant-free methods of producing brain stimulation have been developed, but were limited by spatial resolution or access. Other magnetic approaches studied needed genetic modifications to work, ruling it out for humans.
Since all nerve cells are sensitive to electrical signals, Kim, a graduate student in Anikeeva’s group, hypothesised that a magnetoelectric nanomaterial that can efficiently convert magnetisation into electrical potential could offer a path toward remote magnetic brain stimulation.
To this end, the researchers created nanodiscs with a magnetic core and piezolectric shell. When the core was squeezed by a magnetic field, strain in the shell produces a varying electrical polarisation. This enables the particles to deliver electrical pulses to neurons. The disc shape enhances the magnetostriction effect more than 1000-fold compared to spherical particles used previously.
After testing the nanodiscs with neurons in vitro, the researchers then injected small droplets of nanodisc-bearing solution into specific regions of the brains of mice. With an electromagnet, they turned on and off the stimulation in that region. That electrical stimulation “had an impact on neuron activity and on behaviour,” Kim says.
The team found that the magnetoelectric nanodiscs could stimulate a deep brain region, the ventral tegmental area, that is associated with feelings of reward.
The team also stimulated another brain area, the subthalamic nucleus, associated with motor control. “This is the region where electrodes typically get implanted to manage Parkinson’s disease,” Kim explains. The researchers were able to successfully demonstrate the modulation of motor control through the particles. Specifically, by injecting nanodiscs only in one hemisphere, the researchers could induce rotations in healthy mice by applying magnetic field.
The nanodiscs could trigger the neuronal activity comparable with conventional implanted electrodes delivering mild electrical stimulation. The authors achieved subsecond temporal precision for neural stimulation with their method yet observed significantly reduced foreign body responses as compared to the electrodes, potentially allowing for even safer deep brain stimulation.
The multilayered chemical composition and physical shape and size of the new multilayered nanodiscs is what made precise stimulation possible.
While the researchers successfully increased the magnetostrictive effect, the second part of the process, converting the magnetic effect into an electrical output, still needs more work, Anikeeva says. While the magnetic response was a thousand times greater, the conversion to an electric impulse was only four times greater than with conventional spherical particles.
“This massive enhancement of a thousand times didn’t completely translate into the magnetoelectric enhancement,” says Kim. “That’s where a lot of the future work will be focused, on making sure that the thousand times amplification in magnetostriction can be converted into a thousand times amplification in the magnetoelectric coupling.”
Further work is need before studies involving humans can begin, Kim says.
Source: MIT