CRISPR ‘Molecular Scissors’ can Leave Gaping Holes in the Chromosome
The CRISPR molecular scissors have the potential to revolutionise the treatment of genetic diseases. This is because they can be used to correct specific defective sections of the genome. Unfortunately, there is a catch: under certain conditions, the repair can lead to new genetic defects – as in the case of chronic granulomatous disease. This was reported in the journal Communications Biology by a team from the University of Zurich (UZH).
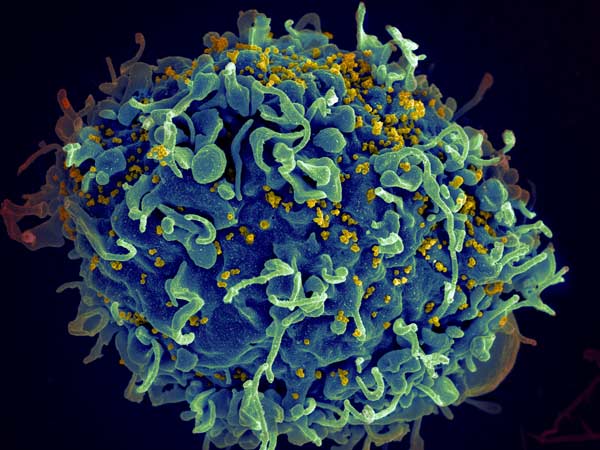
Chronic granulomatous disease is a rare hereditary disease that affects about one in 120 000 people. The disease impairs the immune system, making patients susceptible to serious and even life-threatening infections. It is caused by the absence of two letters, called bases, in the DNA sequence of the NCF1 gene. This error results in the inability to produce an enzyme complex that plays an important role in the immune defence against bacteria and moulds.
The CRISPR tool works…
The research team has now succeeded in using the CRISPR system to insert the missing letters in the right place. They performed the experiments in cell cultures of immune cells that had the same genetic defect as people with chronic granulomatous disease. “This is a promising result for the use of CRISPR technology to correct the mutation underlying this disease,” says team leader Janine Reichenbach, professor of somatic gene therapy at the University Children’s Hospital Zurich and the Institute for Regenerative Medicine at UZH.
… but unfortunately, it’s not perfect
Interestingly however, some of the repaired cells now showed new defects. Entire sections of the chromosome where the repair had taken place were missing. The reason for this is the special genetic constellation of the NCF1 gene: it is present three times on the same chromosome, once as an active gene and twice in the form of pseudogenes. These have the same sequence as the defective NCF1 and are not normally used to form the enzyme complex.
CRISPR’s molecular scissors cannot distinguish between the different versions of the gene and therefore occasionally cut the DNA strand at multiple locations on the chromosome – at the active NCF1 gene as well as at the pseudogenes. When the sections are subsequently rejoined, entire gene segments may be misaligned or missing. The medical consequences are unpredictable and, in the worst case, contribute to the development of leukaemia. “This calls for caution when using CRISPR technology in a clinical setting,” says Reichenbach.
Safer method sought
To minimise the risk, the team tested a number of alternative approaches, including modified versions of CRISPR components. They also looked at using protective elements that reduce the likelihood of the genetic scissors cutting the chromosome at multiple sites simultaneously. Unfortunately, none of these measures were able to completely prevent the unwanted side effects.
“This study highlights both the promising and challenging aspects of CRISPR-based therapies,” says co-author Martin Jinek, a professor at the UZH Department of Biochemistry. He says the study provides valuable insights for the development of gene-editing therapies for chronic granulomatous disease and other inherited disorders. “However, further technological advances are needed to make the method safer and more effective in the future.”
Source: University of Zurich